Tetanus is a serious bacterial infection that affects the nervous system and causes muscles throughout the body to tighten (painful muscle spasms). It’s also called lockjaw because the infection often causes muscle contractions in the jaw and neck.
However, it can eventually spread to other parts of the body. The bacterium, clostridium tetani (C. Tetani), has been implicated as the causative agent for Tetanus.
C. tetani is a slender, gram-positive, anaerobic rod that may develop a terminal spore, giving it a drumstick appearance. The organism is sensitive to heat and cannot survive in the presence of oxygen.
The spores, in contrast, are very resistant to heat and the usual antiseptics. They can survive autoclaving at 249.8°F (121°C) for 10–15 minutes. The spores are also relatively resistant to phenol and other chemical agents. Autoclaving is the method used in sterilizing hospital equipment.
The spores are widely distributed in the soil and the intestines and faeces of horses, sheep, cattle, dogs, cats, rats, guinea pigs, and chickens. Manure-treated soil may contain large numbers of spores. In agricultural areas, a significant number of human adults may harbour the organism.
The spores can also be found on skin surfaces and in contaminated heroin. (Heroin users, particularly persons who inject themselves subcutaneously, appear to be at high risk for tetanus. Quinine is used to dilute heroin and this supports the growth of C. tetani).
Although tetanus affects people of all ages; however, the highest prevalence is seen in newborns and young persons. C. tetani produces two exotoxins viz:
- Tetanolysin.
The function of tetanolysin is not known with certainty.
- Tetanospasmin.
Tetanospasmin is a neurotoxin and causes the clinical manifestations of tetanus. Based on weight, tetanospasmin is one of the most potent toxins known. The estimated minimum human lethal dose is 2.5 nanograms per kilogram of body weight (a nanogram is one billionth of a gram) or 175 nanograms for a 70-kg (154lb) human.
C. tetani usually enters the body through a wound. In the presence of anaerobic (low oxygen) conditions, the spores germinate. Toxins are produced and disseminated via blood and lymphatics.
Toxins act at several sites within the central nervous system, including peripheral motor end plates, the spinal cord, and the brain, and the sympathetic nervous system. The typical clinical manifestations of tetanus are caused when tetanus toxin interferes with the release of neurotransmitters, blocking inhibitor impulses.
This leads to unopposed muscle contraction and spasms. Seizures may occur, and the autonomic nervous system may also be affected.
What then is tetanus?
Tetanus is an acute poisoning from a neurotoxin (toxins that are destructive to nerve tissue). Produced by a bacterium, clostridium tetani and it is characterized by an acute onset of increased muscle tone (hypertonia), painful muscular contractions (usually of the muscles of the jaw and neck), and generalized muscle spasms without other apparent medical causes.
It’s often referred to as “lockjaw” because it can cause painful spasms and stiffness in your jaw muscles. Worldwide, tetanus is estimated to cause over 200,000 deaths annually, mostly in neonates and young children, but the disease is so rarely reported that all figures are only rough estimates.
Transmission is primarily by contaminated wounds (apparent and inapparent). The wound may be major or minor. In recent years, however, a higher proportion of patients had minor wounds, probably because severe wounds are more likely to be properly managed.
Tetanus may follow elective surgery, burns, deep puncture wounds, crush wounds, otitis media (ear infections), dental infection, animal bites, abortion, and pregnancy or after childbirth in the uterus (maternal tetanus) and a neonate’s umbilicus (tetanus neonatorum) as a result of unsanitary delivery and umbilical cord care practices.
Diabetes and a history of immunosuppression may be risk factors for tetanus. Tetanus is not contagious from person to person. It is the only vaccine-preventable disease that is infectious but not contagious.
Classifications
Based on clinical findings, three different forms of tetanus have been described.
-
Local tetanus
This is an uncommon form of the disease, in which patients have persistent contraction of muscles in the same anatomic area as the injury. These contractions may persist for many weeks before gradually subsiding.
Local tetanus may precede the onset of generalized tetanus but is generally milder. Only about 1% of cases are fatal.
-
Cephalic tetanus
Cephalic tetanus is a rare form of the disease, occasionally occurring with otitis media (ear infections) in which
C. tetani is present in the flora of the middle ear, or following injuries to the head.
There is the involvement of the cranial nerves, especially in the facial area. The most common type (about 80%) of reported tetanus is generalized tetanus.
-
Neonatal tetanus
This is a form of generalized tetanus that occurs in newborn infants. Neonatal tetanus occurs in infants born without protective passive immunity because the mother is not immune. It usually occurs through infection of the unhealed umbilical stump, particularly when the stump is cut with an unsterile instrument.
Signs and symptoms
The incubation period (time from exposure to illness) ranges from 3 to 21 days, usually about 8 days. In general, the further the injury site is from the central nervous system, the longer the incubation period.
The shorter the incubation period, the higher the chance of death. In neonatal tetanus, symptoms usually appear from 4 to 14 days after birth, averaging about 7 days. The disease usually presents with a descending pattern viz:
- The first sign is trismus or lockjaw (Jaw stiffness).
- Risus sardonicus (rigid smile because of sustained contraction of facial musculature).
- Neck Stiffness.
- Difficulty in swallowing.
- The rigidity of abdominal muscles.
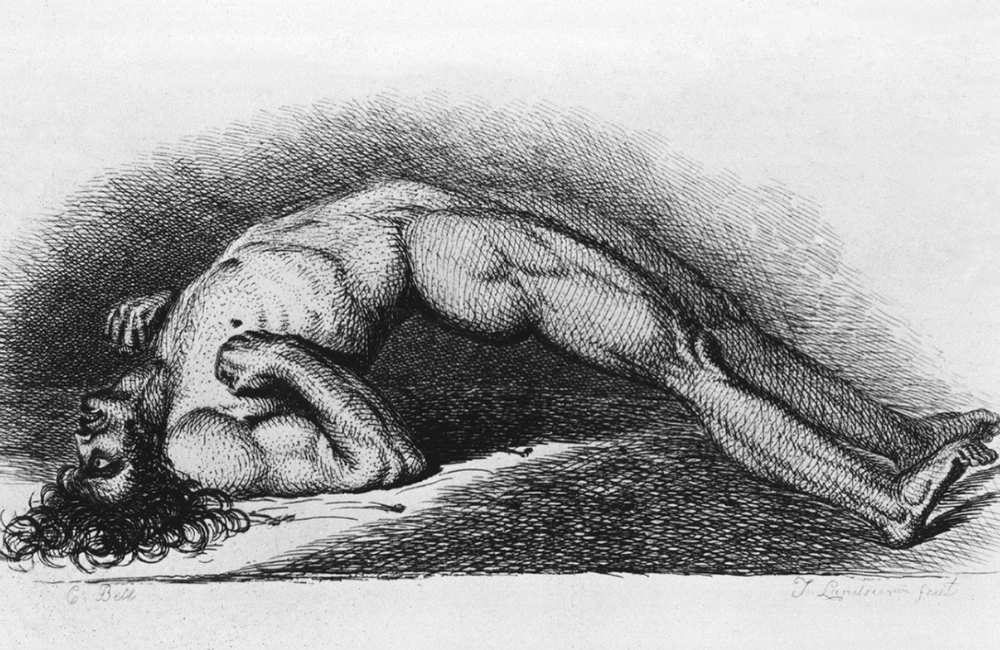
- Arching of the back (opisthotonos).
- Autonomic instability can also occur in these patients and they include:
-
- Fever (Elevated temperature.)
- Dysrhythmia.
- Labile blood pressure and heart rate.
- Respiratory difficulties.
- Catecholamine excretion (sweating, headache.
- Early death.
- Other symptoms include
-
- Sore throat.
- Tonic spasms.
- Restlessness
- Irritability
- Spasms may occur frequently and last for several minutes. Spasms continue for 3–4 weeks. Complete recovery may take months.
Investigations of tetanus
There are no laboratory investigations for tetanus. The diagnosis is entirely clinical and does not depend upon bacteriologic confirmation.
C. tetani can sometimes be cultured from the wound, but culture is not sensitive; only 30% of patients with tetanus have positive cultures. Also, false-positive cultures can occur in patients without tetanus.
Diagnosis
The diagnosis is entirely clinical. Tetanus should be considered when patients have sudden, unexplained muscle stiffness or spasms, particularly if they have a history of a recent wound or risk factors for tetanus.
Tetanus can be confused with meningoencephalitis of bacterial or viral origin, but the following combination suggests tetanus:
- An intact sensorium.
- Normal cerebrospinal fluid.
- Muscle spasms.
Trismus must be distinguished from a peritonsillar or retropharyngeal abscess or another local cause. Phenothiazines can induce tetanus-like rigidity (e.g., dystonic reaction, neuroleptic malignant syndrome).
Treatment of tetanus
Treatment of tetanus can be subdivided into the following viz:
-
Supportive care
-
- The patient should be kept in a quiet room.
- In moderate or severe cases, patients should be intubated and adequate ventilation is maintained thus mechanical ventilation becomes essential when the neuromuscular blockade is required to control muscle spasms that impair respiration.
- Continuous nursing care.
- Fluid balance should be maintained.
- Intravenous(iv) hyperalimentation (artificial supply of nutrients typically intravenously) avoids the hazard of aspiration secondary to gastric tube feeding. Because constipation is usual, stools should be kept soft. A rectal tube may control distention.
Bladder catheterization is required if urinary retention occurs.
-
- Intravenous magnesium has been shown to prevent muscle spasms.
It should be given IV in the form of a bolus of 5 g followed by a continuous infusion at a rate of 2-3 g/hour until the spasm control has been achieved. During magnesium infusion, the patellar reflex needs to be monitored. If areflexia develops, the dose should be reduced. Areflexia is the absence of deep tendon reflexes.
-
- Chest physiotherapy.
Frequent turning and forced coughing are essential to prevent pneumonia. Analgesia with opioids is often needed.
-
Wound care
Because dirt and dead tissue promote C. tetani growth, prompt, thorough debridement, especially of deep puncture wounds, is essential to prevent further toxin release. Antibiotics are not substitutes for adequate debridement.
-
Tetanus antitoxin and toxoid
Early and adequate use of human tetanus immune globulin (HTIG) to neutralize nonfixed toxins and prevention of further toxin production is advised. HTIG does not affect the toxin that is already bound to the central nervous system.
It also shortens the course of illness and may help in reducing the severity. For adults, human HTIG 3000 to 6000 units IM is given once, split and given at separate sites around the wound. Antitoxin and vaccine should be injected into different body sites to avoid neutralizing the vaccine.
Antitoxin of animal origin is far less preferable because it does not maintain the patient’s serum antitoxin level well and the risk of serum sickness is considerable. If horse serum must be used, the usual dose is 50,000 units intramuscularly or intravenously (usually skin testing is done).
-
Management of muscle spasms
Benzodiazepines are the standard of care to control rigidity and spasms. Diazepam can help control seizures, counter muscle rigidity, and induce sedation. Midazolam is water-soluble and it is preferred for prolonged therapy because it reduces the risk of lactic acidosis and long-acting metabolites accumulating and causing coma.
-
Antibiotics
The role of antibiotic therapy is minor compared with wound debridement and general support. Typical antibiotics include:
-
- Penicillin G 6 million units IV every 6 hours.
- Doxycycline 100 mg IV 2 times a day.
- Metronidazole 500 mg IV every 6 to 8 hours.
Although toxins are the main cause of disease, metronidazole has been shown to slow the progression of the disease and has been shown to decrease mortality as well.
-
Management of autonomic dysfunction
-
- Morphine may be given every 4 to 6 hours to control autonomic dysfunction, especially cardiovascular.
- Beta-blockade is used to control episodes of hypertension and tachycardia. Please note that sudden cardiac death is a feature of tetanus, and beta-blockade can increase risk; however, esmolol, a short-acting beta-blocker, has been used successfully. (Do not use propranolol).
Tetanus Prevention
Tetanus infection does not confer immunity, so unless their vaccination history indicates completion of a full primary series, patients should receive a full primary tetanus vaccination thus being up to date with your vaccine is the best tool to prevent tetanus.
The vaccine usually is given to children as part of diphtheria and tetanus toxoids and acellular pertussis (DTaP) vaccine. This vaccination protects against three diseases: throat and respiratory infection (diphtheria), whooping cough (pertussis), and tetanus.
All women who become pregnant should receive the vaccine during the pregnancy (and any following pregnancies). This reduces the risk of neonatal tetanus infection by 94 per cent.
Puncture wounds or other deep cuts, animal bites, or particularly dirty wounds put you at increased risk of tetanus infection. Seek medical attention if the wound is deep and dirty, particularly if you’re unsure of when you were last vaccinated. Leave unclean wounds open to avoid trapping bacteria in the wound with a bandage.
If a contraindication to using tetanus toxoid-containing preparations exists, passive immunization with tetanus immune globulin (TIG) should be considered whenever an injury other than a clean minor wound is sustained.
What are the complications of tetanus?
Complications can include:
- Uncontrolled or involuntary tightening of the vocal cords (laryngospasm).
- Broken bones due to severe muscle spasms.
- Joint dislocation.
- Breathing problems.
- Pneumonia.
- High blood pressure or abnormal heart rhythms.
- Pulmonary embolism (blood clot in the lung).
- Infections acquired by a patient during a hospital visit (nosocomial infections).
- Paralytic ileus
- Pressure sores
- Stress ulcers
- Coma
- Nerve palsy
- Urine retention
- Seizures
- Death.
Respiratory failure is the most common cause of death. Laryngeal spasms and rigidity and spasms of the abdominal wall, diaphragm, and chest wall muscles cause asphyxiation.
Hypoxemia can also induce cardiac arrest, and pharyngeal spasm leads to aspiration of oral secretions with subsequent pneumonia, contributing to a hypoxemic death.
Pulmonary embolism is also possible. However, the immediate cause of death may not be apparent.
Conclusion
Tetanus is a potentially deadly disease of the central nervous system that can be prevented by a vaccine. The recovery is slow and it can take months. Both neonatal and cephalic tetanus have poor prognoses.
Even those who survive to need tetanus toxoid as the infection does not confer immunity. If you suspect you may have been exposed to tetanus, see your doctor for immediate medical attention.