Stroke, medically referred to as, a cerebrovascular accident (CVA), is a serious life-threatening medical emergency that occurs when blood flow to a part of the brain is interrupted as a result of a broken or blocked blood vessel. Brain cells that do not receive a constant supply of oxygenated blood may die, causing permanent damage to the brain.
It is one of the leading causes of morbidity and mortality worldwide. WHO statistics indicate that stroke is the third leading cause of death (13-15%) after heart disease and cancer.
Each year about 15 million persons suffer from stroke worldwide out of which 5 million end up with mortality and the remaining 10 million will be deeply disabled.
Definition of Stroke
A stroke is an acute focal neurological deficit caused by a vascular lesion of sudden onset with the symptoms lasting longer than 24 hours if the patient survives.
Types of Stroke
There are 2 types of acute strokes in adult patients.
-
Ischemic Stroke (Cerebral Infarction)
Here, there is an acute focal neurological deficit caused by a sudden onset blockage of vascular supply in the local region of the brain or during general circulatory failure due to cardiac arrest and systemic hypotension.
Occlusion of the cerebral artery typically results in an area (the “core”) so severely lacking blood supply (ischemia) that will be damaged irreversibly within minutes or hours, surrounded by a less ischemic penumbra of neuronal tissue that may be temporarily inactivated.
The ischemic penumbra can be defined as a functionally impaired and severely ischemic area; consisting of potentially surviving brain tissue that is at risk of losing blood supply but that can recover if its blood supply is reestablished on time.
If the occluded artery reopens early and sufficiently with subsequent improvement or normalization of the blood supply, the ischemic area will be small or absent and its clinical expression might well be a transient Ischemic attack (TIA) see below and there is a complete clinical recovery.
Ischemic Stroke (Cerebral Infarction) is divided into sub-groups viz:
-
- Embolic stroke
Occurs when a blood clot from the heart (cardioembolic) or another blood vessel (artery-to artery embolism) breaks and occludes more distal artery supply to the brain.
-
- Lacunar infarct
Clogged arteries: Fat, cholesterol and other substances can collect on the walls of blood vessels. Over time, these substances harden and form structures called plaque. The build-up of fat deposits and plaque clogs arteries, narrowing the passageway for blood.
-
- Hemodynamic infarct
Here there is evidence of flow failure caused by severe narrowing or occlusion of a large artery.
-
- Transient ischemic attack (TIA)
This is a temporary episode of focal ischemic neurologic dysfunction that completely resolves within 24 hours.
-
- Reversible ischemic neurologic deficit (RIND)
This is also called a minor stroke and is considered when a focal ischemic deficit persists for longer than 24 hours but resolves within 3 weeks.
-
- Progressing cerebral infarction
Is considered when rapid evolution of ischemic cerebral vascular events occurs in patients who have increasing neurologic deficit for as long as 72 hours after the onset of symptoms. This syndrome is more common in the territory of the vertebrobasilar system.
-
Intracerebral Hemorrhages
A hemorrhagic stroke occurs when a blood vessel in the brain ruptures or breaks, allowing blood to leak into the brain most likely secondary to chronic hypertension
-
- Aneurysmal Subarachnoid Hemorrhage
Subarachnoid haemorrhage is spontaneous arterial bleeding into the subarachnoid space of the brain caused by a rupture of the arterial aneurysm.
Causes of Cerebral Infarctions
There are three leading causes of cerebral infarcts namely:
- Extra- and intracranial large artery disease
- Cardio embolism(a blood clot from the heart)
- Small artery disease (microangiopathy)
About one-third of the sources remain undiagnosed even if carefully investigated.
Stroke Symptoms
Recognizing the sign and symptoms is critical to early intervention and treatment. The symptoms depend on which parts of your brain are affected. They can include things like:
- Sudden numbness or weakness of your face, arm, or leg, often on one side of the body.
- Confusion.
- Problems speaking or understanding others.
- Dizziness, loss of balance or coordination, or trouble walking.
- Vision loss or double vision.
Diagnosing Stroke
The Face, Arm, Speech Tests (FAST) for Stroke Diagnosis was developed in 1998 as a stroke identification tool that examines facial weakness, arm weakness, and speech disturbance and allows paramedics to quickly identify stroke and accurately. Researchers found that paramedics who used the Face Arm Speech Test (FAST) were in close agreement with neurologists using the National Institute of Health Stroke Scale in early recognition of this illness.
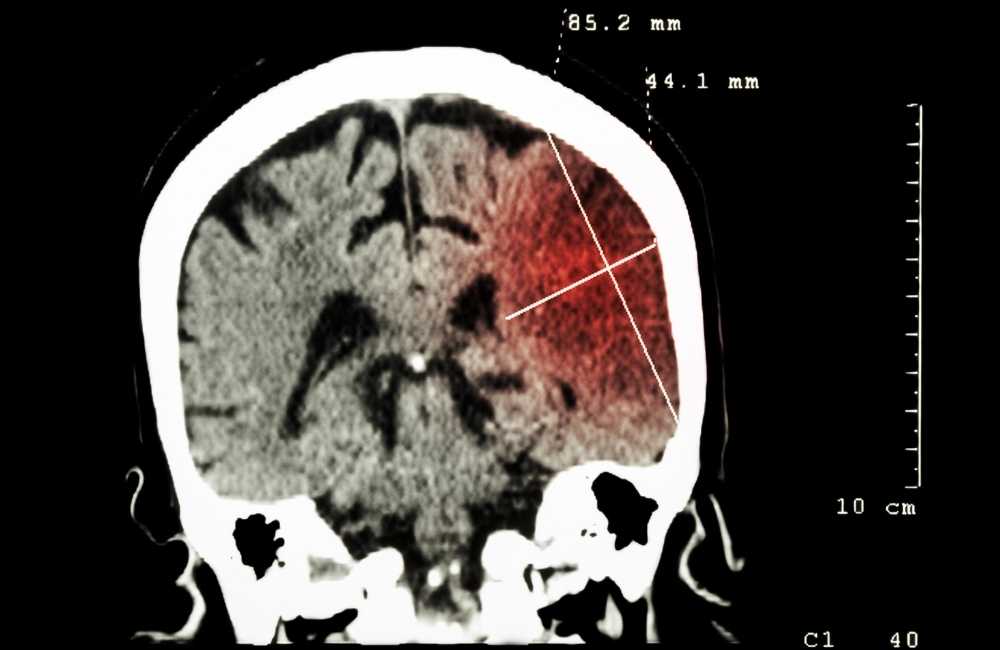
The first step in assessing a patient is to determine whether the patient is experiencing an ischemic or hemorrhagic stroke so that the correct treatment can begin. A Brain CT scan or MRI is typically the first test performed.
Investigations for Stroke
-
A Physical Exam
Your doctor will do several tests you’re familiar with, such as listening to the heart and checking the blood pressure. You’ll also have a neurological exam to see how a potential stroke is affecting your nervous system.
-
Blood Tests
You may have several blood tests.
-
- Complete blood count and platelet count.
- Prothrombin time or INR,
- Partial Thrombin Time (PTT).
- Serum electrolytes.
- Blood glucose.
- C-reactive protein (CRP).
- Erythrocyte Sedimentation rate(ESR).
- Hepatic and renal chemical analysis.
-
Imaging

-
- Computerized tomography (CT) scans
A CT scan uses a series of X-rays to create a detailed image of the brain. CT-scan can show bleeding in the brain, ischemic stroke, tumour or other conditions.
-
- CT-Angiography (CTA)
May be performed. In CTA, a contrast may be injected intravenously and images are obtained of the cerebral blood vessels. Images that detect blood flow, called CT perfusion (CTP) may be obtained at the same time. This procedure gives a detailed view of arteries in the brain and neck. The combination of CT, CTA and CTP can help the Doctor decide on the best therapy for the patient.
-
- Magnetic Resonance Imaging (MRI)
An MRI uses powerful radio waves and a magnetic field to create a detailed view of the brain. An MRI can detect brain tissue damaged by an ischemic stroke and brain haemorrhages. Your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow (magnetic resonance angiography or magnetic resonance venography).
-
- Carotid Ultrasound / Doppler Ultrasound
In this test, sound waves create detailed images of the inside of the carotid arteries in the neck. This test shows the buildup of fatty deposits (plaques) and blood flow in the carotid arteries.
-
- Echocardiogram (ECG, EKG)
An electrocardiogram checks the heart’s electrical activity, this can help determine whether heart problems caused the stroke.
Treatment for Stroke
Any patient suspected of having a stroke should be transported as quickly and safely as possible to the nearest hospital with staff experienced in acute stroke management and emergency brain imaging. The emergency aid to such patients can be taken in a short time in the following orders:
-
Pre-hospital recognition of stroke symptoms
Once a stroke is suspected, establish time zero – the time when the patient was last known to be neurologically normal. If the patient was sleeping and woke up with symptoms, time zero is the last time the patient was seen to be normal, then arrange to move to a stroke centre.
-
Transportation to the hospital with a stroke unit
Within 10 minutes (Time goal) of the patient’s arrival in the emergency department the following actions should be taken:
- Airway, Breathing and Circulation assessment (ABC).
- Oxygen administration.
- IV line access should be secured.
- Order for investigations, Brain CT-scan and ECG or EKG.
-
Evaluation of general condition and neurological status of patients in a stroke unit
Within 25 minutes of the patient’s arrival, the following actions should be taken:
- History Review.
- Physical examination/Neurological examination.
- Brain CT was completed and results in 45 minutes.
- Establish Neurological and CT diagnosis and immediate starting of general and specific appropriate treatment.
Treatment depends on the type of stroke; immediate treatment can help save lives and reduce disability by restoring blood flow for an ischemic stroke or controlling bleeding and reducing pressure on the brain in the case of a hemorrhagic stroke.
Non-Surgery
If a stroke is caused by a blood clot, the patient may be able to receive a clot-busting drug such as a tissue plasminogen activator (T-PA) to dissolve the clot and help restore blood flow to the damaged area of the brain.
Clot-busting drugs, which can only be given within the first few hours of stroke onset, are typically delivered intravenously by emergency medical personnel or in the hospital emergency department.
Patients may also receive blood-thinning drugs such as Aspirin, warfarin, heparin or clopidogrel.
Surgery
Surgery to remove blood from around the brain and repair damaged blood vessels.
- Endovascular therapy
This is a minimally invasive intracranial vascular procedure used in improving blood flow in the brain’s arteries and veins. In endovascular therapy, an image-guided catheter is navigated through the body’s blood vessels to the brain to deliver:
- Drugs to dissolve the clot.
- Mechanical retrievers and aspiration systems remove blood clots or debris in cerebral arteries.
- To insert devices, like balloons which are used to open markedly narrowed blood vessels -a balloon-tipped catheter is guided to where the artery is narrow or blocked and inflated to open the vessel and stents (a small wire mesh tube) may be placed in the artery to help keep it open.
Post-Treatment Rehabilitation
Following a stroke, many patients will receive post-stroke rehabilitation to overcome disabilities that may occur as a result of the stroke. Post-stroke treatment may also include efforts to prevent another stroke by controlling or eliminating risk factors such as high blood pressure, high cholesterol and diabetes.
Every person’s stroke recovery is different. Depending on the condition, the treatment team may include a chain of specialists, ranging from Neurologists to clerics.
Conclusion
The “7 D’s of Stroke Care” highlight the major steps in diagnosis and treatment viz
- Detection.
- Dispatch.
- Delivery.
- Door (arrival and urgent triage in the emergency department [ED]).
- Data.
- Decision.
- Drug administration.
The goal of stroke care is to minimize brain injury and maximize patient recovery. The community-oriented “Stroke Chain of Survival” that links actions to be taken by patients, family members, and healthcare providers to maximize stroke recovery are the following:
- Rapid recognition and reaction to stroke warning signs.
- Rapid emergency medical services (EMS) dispatch.
- Rapid EMS system transport and hospital pre-notification.
- Rapid diagnosis and treatment in the hospital.
- Rehabilitation.
- Primary prevention.
- Secondary prevention.

