Recurrent vulvovaginal candidiasis (RVVC) can only be fully understood if we learn about thrush itself. About 75 % of women suffer from uncomplicated vaginal candidiasis once in their lifetime while recurrent vulvovaginal candidiasis occurs in less than 5 % of women.
Normal Thrush
Vaginal thrush is caused by a yeast called Candida Albicans – It’s an organism that usually lives in the gut and the vagina and is responsible for 85-95% of vaginal yeast infections. Also, other Candida species have been implicated e.g.
- Candida Tropicalis
- Candida Glabrata
Causes of Thrush
Candida can occur for no obvious reasons but the following well-recognised factors have been noted.
- Antibiotics
It is an observation that women treated with broad-spectrum antibiotics develop vaginal thrush.
- Sexual intercourse
Vaginal thrush is not considered a Sexually transmitted infection(STI) but a strong association with sexual exposure has been reported.
- Oral sex
Frequent receptive oral-genital contact increases the risk of vaginal thrush.
- Decreased immunity states
This increases susceptibility to vaginal thrush as Seen in people with HIV/AIDS or persons taking steroids or cancer drugs.
- Diabetes (DM)
Vaginal thrush is very common in women with DM especially when off control.
- Pregnancy, Hormone Replacement Therapies and Combined Oral
Contraceptives especially those with very high estrogen levels are known risk factors.
Other Factors that Can Cause Thrush
- Wearing tight and nylon underwear with inadequate ventilation.
- Vaginal Douching or wash.
- Use of feminine deodorants.
- Using deodorant (scented) tampons or pads.
- Sharing of fomites.
- Use of an intrauterine device.
- Use of Bubble Bath.
Symptoms of Thrush
- Vaginal itching.
- Burning and sore vagina.
- White, curd-like, non-offensive vaginal discharge.
- Painful sex.
- Pain on urination.
On clinical examination, you see a dry, fissured and red vulva with a white curd-like discharge adhering to the vagina walls or cervix.
Investigations for Thrush & Recurrent VulvoVaginal Candidiasis
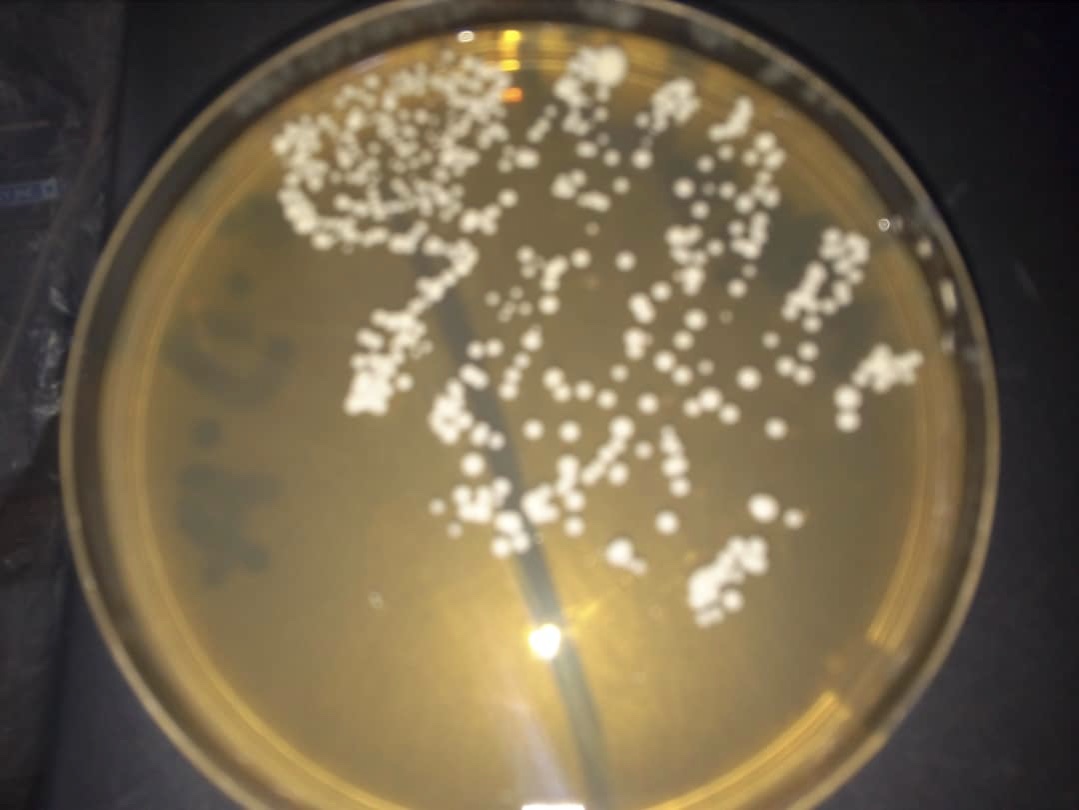
Plate showing growth of Candida
-
Vaginal microscopy and culture
An acute infection is confirmed by the presence of candida pseudo hyphae or budding yeast forms on microscopy but culture is the most sensitive method of detecting candida spp. The presence of >10 yeast colonies is diagnostic of Candida.
-
Vaginal pH
PH is the measure of acidity. The normal PH of the vagina is between 3.5 to 4.5. This is created by the organism that normally lives in the vagina, the Doderlein bacillus, it feeds on the glycogen stores in the vagina thus releasing Lactic acid, which is responsible for vaginal acidity, therefore it can be said that the vagina is slightly acidic.
An alkaline shift in vaginal PH to up to PH 5 favours the growth of fungus and bacteria causing vaginal infection (Bacterial Vaginosis) or TricomonasVaginalis
Treatment for Thrush
Treatment is anti-fungal preparations.
- A topical-clinical cure is achieved in about 80% although should be used in conjunction with the pessaries(or Vaginal Tablets)
-
- Clorimazole 1%
- Econazole 1%
- Miconazole 2%
- Pessariesor Vaginal tabs
- Oral Tablets
-
- Fluconazole
- Itraconazole
What is Recurrent VulvoVaginal Candidiasis (RVVC)?
The occurrence of four episodes or more of candidiasis per year that is mycologically proven is called recurrent vulvovaginal candidiasis (RVVC)
Causes of Recurrent Thrush VulvoVaginal Candidiasis
- Immunosuppression
E.g. HIV/AIDS
- Vaginal relapse
Incompletely eradicated candida from the vagina with previous antifungal treatment.
- Changes in fungal virulence
- Women with Lewis blood group
These groups of women are more susceptible to vaginal colonization with Candida.
- Psychological problems
Indirect evidence shows that psychological problems contribute to the incidence of RVVC. Depression, helplessness, hopelessness, and stressful life events may lead to the disease by inhibiting the immune systems of individuals.
Treatment for Recurrent Thrush VulvoVaginal Candidiasis (RVVC)
This is difficult to treat, but careful history and knowledge of previous antifungal preparations are key to an accurate diagnosis.
The patient’s symptoms are usually worse before the period and feel better after menstruation.
-
General Measures Against Recurrent VulvoVaginal Candidiasis
-
- Prophylactic antifungals should be given to women who develop antibiotic thrush with further antibiotic courses.
- Avoid local irritants such as bubble baths, perfumed soap or Tampons.
- Tightly fitting garments should be discouraged.

-
Drug That Can Treat Recurrent VulvoVaginal Candidiasis
Longer courses of antifungal may be required with maintenance dose continuing for up to 6 months or more.
-
- Fluconazole 100mg weekly
- Ketoconazole 100mg per day
- Clotrimazole pessaries 500mg weekly
Treatment of Sexual Partner
Asymptomatic sexual partners are often given antifungals but there is no evidence that it benefits the women.
Conclusion
Recurrent vulvovaginal candidiasis (RVVC) affects the quality of life, romantic relationships, and sexual performance (with less sexual satisfaction/less orgasm).
Also, there is evidence that psychological problems (Depression, anxiety and stress in the past four weeks are related to an increased risk of RVVC. Therefore, in addition to drug treatment, psychological interventions and sexual counselling can be effective in improving RVVC.

