Pneumonia is a lower respiratory lung infection that causes an acute inflammation of one or both lungs, typically due to a bacterial, viral, or fungal infection.
The tiny air sacs, called the alveoli, inside the lungs get filled with fluid or pus thus causing symptoms such as coughing, chest pain, and breathing difficulties which can deteriorate leading to hospitalization.
Children are at greater risk of contracting the disease because their immune systems aren’t fully developed. It can progress very quickly in children, particularly infants and those with underlying medical conditions
Pneumonia is classed as follows:
- Lobar pneumonia
Each lung is made of lobes, which are defined sections of the lung. It affects one or more lobes of your lungs.
- Bronchial pneumonia
It is also known as bronchopneumonia. It affects patches throughout both lungs.
Symptoms of Pneumonia
The symptoms can be mild to life-threatening. They can include:
- Cough that may produce Phlegm (mucus).
- Fever.
- Sweating or Chills.
- Shortness of breath that happens while doing normal activities, or even while resting.
- Chest Pain that’s worse when you breathe or cough.
- Feelings of tiredness or fatigue.
- Loss of appetite.
- Nausea or vomiting.
- Confusion, particularly in older people.
- Headaches.
Categorisation of Pneumonia
It can be categorized into the following. See below. Please note that these categorizations allow treatment to be selected empirically.
-
Community – acquired
It is the most common type. It occurs outside of hospitals or other healthcare facilities. It may be caused by: bacteria, viruses, and fungi. Pathogens vary by patient age and other factors.
-
- Bacterial causes
The most common cause of bacterial pneumonia is Streptococcus pneumonia. This type can occur on its own or after a cold or the flu. It may affect one part (lobe) of the lung, a condition called lobar pneumonia.
-
- Bacteria-like organisms
Mycoplasma pneumonia also can cause pneumonia. It typically produces milder symptoms than other types. Walking pneumonia is an informal name given to this type, which typically isn’t severe enough to require bed rest.
-
- Viral causes
Viruses, including COVID-19 and some of the viruses that cause colds and the flu can cause pneumonia. Viruses are the most common causes in children younger than 5 years.
Viral pneumonia is usually mild. But in some cases, it can become very serious. Coronavirus 2019 (COVID-19) may cause pneumonia, which can become severe.
-
- Fungi
This type is most common in people with chronic health problems or weakened immune systems, and in people who have inhaled large doses of the organisms. The fungi that cause it can be found in soil or bird droppings and vary depending on geographic location.
-
Hospital Acquired
Some people catch this illness during a hospital stay for another illness. This type can be serious because the bacteria causing it may be more resistant to antibiotics and because the people who get it are already sick.

-
- Health care-acquired pneumonia
Health care-acquired pneumonia is a bacterial infection that occurs in people who live in long-term care facilities or who receive care in outpatient clinics, including kidney dialysis centers. Like hospital-acquired pneumonia, health care-acquired pneumonia can be caused by bacteria that are more resistant to antibiotics.
-
- Ventilator – Associated
People who are on breathing machines (ventilators), often used in intensive care units, are at higher risk of this type of pneumonia.
-
- Pneumonia Occurring in Immune Compromised Patients
For example Pneumocystis jirovecii pneumonia in HIV infection.
-
- Aspiration Pneumonia
It occurs when large volumes of upper airway or gastric secretions enter into the lungs. E.g.When you inhale food, drink, vomit or saliva into your lungs. Aspiration is more likely if something disturbs your normal gag reflex, such as a brain injury or swallowing problem, or excessive use of alcohol or drugs.
How Does One Get Pneumonia
The airways and lungs are constantly exposed to pathogens in the external environment; the upper airways and oropharynx in particular are colonized with so-called normal flora. Micro aspiration of these pathogens from the upper respiratory tract is a regular occurrence, but these pathogens are readily dealt with by lung host defense mechanisms. Pneumonia develops when
- Defense mechanisms are compromised
-
- Upper Airway defenses
Include salivary IgA, proteases, and lysozyme; growth inhibitors produced by normal flora and fibronectin, which coats the mucosa and inhibits adherence.
-
- Lower airway defenses
Including cough and mucociliary clearance prevent infection in airspaces. Specific lower airway defences include various pathogen-specific immune mechanisms, including IgA and IgG opsonization(A process the immune system uses opsonins,an extra cellular protein, to tag foreign pathogens and mark them for elimination by phagocytes),antimicrobial peptides, anti-inflammatory effects of surfactant, phagocytosis by alveolar macrophages, and T-cell–mediated immune responses. These mechanisms protect most people against infection.
- Macro aspiration leads to a large inoculum of bacteria that overwhelms normal host defenses
- A particularly virulent pathogen is introduced.
Occasionally, infection develops when pathogens reach the lungs via the bloodstream or by contiguous spread from the chest wall or mediastinum. Another recently identified potential pathway of pneumonia development is by the disruption of the micro flora balance in the resident micro biome of the lung.
Numerous conditions alter the normal flora (e.g., systemic illness, under nutrition, hospital exposure, and antibiotic exposure) or impaired defenses (e.g., altered mental status, cigarette smoking, nasogastric or endotracheal intubation, disorders or drugs that suppress the immune system). Pathogens that then reach airspaces can multiply and cause pneumonia.
Risk Factors for Pneumonia
Several risk factors have been implicated in Pneumonia
-
Age
Pneumonia can affect anyone. But the two age groups at highest risk are:
-
- Children who are 2 years old or younger
- People who are age 65 or older
-
Being hospitalized
There is a greater risk of pneumonia if one is in a hospital intensive care unit;and worse still if one is on a machine that helpsmaintain breathing (a ventilator).
-
Chronic disease
One is more likely to get pneumonia if some pre morbidchronic health conditionslike asthma, chronic obstructive pulmonary disease (COPD) or heart disease.
-
Smoking
Smoking damages the body’s natural defenses against the bacteria and viruses that cause pneumonia.
-
Weakened or suppressed immune system
People who have HIV/AIDS, who’ve had an organ transplant, or who receive chemotherapy or long-term steroids are at risk.
Investigations
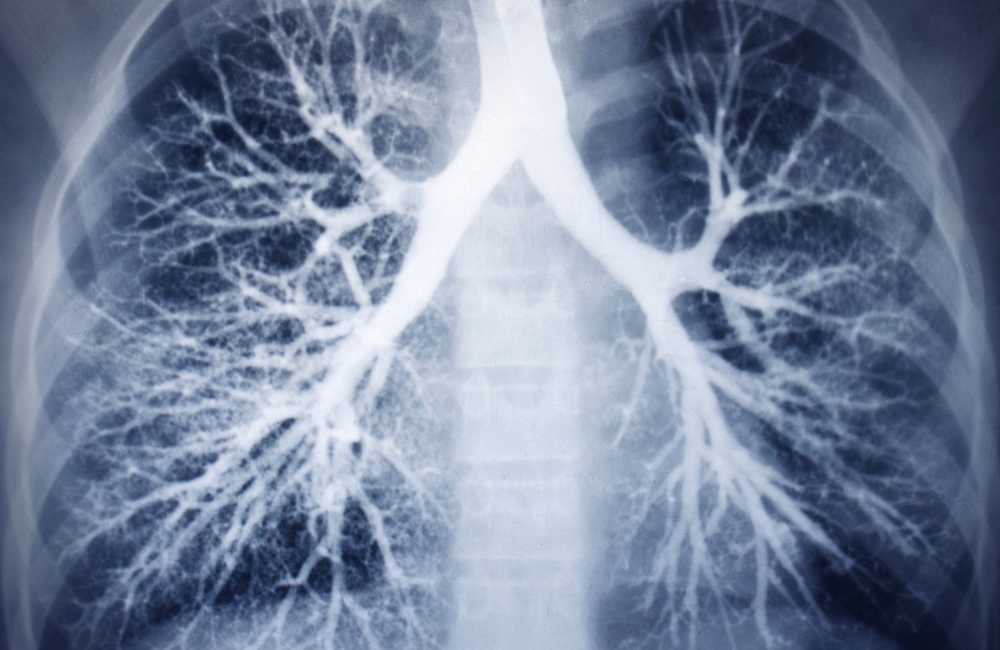
- Chest X-ray
- Complete blood count(CBC)
- Blood culture
This test uses a blood sample to confirm an infection. Culturing can also help identify the organism responsible.
- Sputum culture
During a sputum culture, a sample of mucus is collected after coughing deeply and then sent to a lab to be analyzed to identify the cause of the infection.
- Pulse oximetry
Pulse oximetry measures the amount of oxygen in your blood (oxygen saturation)
- CT scan provides a clearer and more detailed picture of your lungs.
- Fluid sample analysis
If the doctor suspects fluid in the lungs, sample may be taken using a needle placed between your ribs. This test can help identify the cause of your infection.
- Bronchoscopy
Looks into the airways in your lungs. This is done using a camera on the end of a flexible tube that’s gently guided down your throat and into your lungs. The doctor may do this test if initial symptoms are severe, or if patient is hospitalized and not responding well to antibiotics.
Diagnosing Penumonia
Pneumonia diagnosis is based on
-
Medical history
The doctor determines which type of pneumonia you have based on how you became infected, what the X-ray or lung exam reveals, and which kind of organism is responsible for your infection.
-
Physical exam
During a physical exam, the doctor checks the vital signs and listens to the lungs with a stethoscope. Decreased breath sounds is an indication of a lot of inflammation
-
Certain test results
If the doctor suspects pneumonia, some diagnostic tests may be ordered, such as a chest x-Ray to help determine the extent of the infection. Blood work and an analysis of the patient’s sputum can pinpoint what’s causing the pneumonia.
Pulse oximetry measures the oxygen level in the blood (which may be low if pneumonia since the lung is affected). Computerized tomography (CT) scan may be ordered for the elderly, which showsunresolving pneumonia after being treated. This gives a more detail information of the lungs than the chest X-ray.
In severe cases, a pleural fluid culture may also be taken — needle is inserted into the pleural area, between the lungs and the chest wall, to obtain a fluid sample, which is then analyzed to help figure out what’s causing the infection.
Treatment for Pneumonia
Pneumonia treatment depends on the type of pneumonia, how severe it is, and the patient’s general health.
-
Prescription medications
Medication may be prescribed depending on the specific cause of the pneumonia.
-
- Antibiotics
Oral antibiotics canbe used in treating most cases of bacterial pneumonia. Please, note that the entire course of antibiotics have to be taken, even if you begin to feel better.
Depending on the severity of the pneumonia, parenteral antibiotics may be deployed.
-
- Antiviral
However, many cases of viral pneumonia clear on their own with at-home care.
-
- Antifungal
Anti-fungal drugs are used to treat fungal pneumonia. These medications are usually taken for several weeks before clearance is achieved.
-
Hospitalization
If the symptoms are very severe and they’re other co-morbidities, hospitalization may be an option. At the hospital, the vital signs are closely monitored and other treatment may include:
- Intravenous antibiotics.
- Respiratory Therapy
Here specific medications can directly be introduced into the lungs, or patient can be taught how to perform breathing exercises to maximize oxygen usage.
- Oxygen to maintain oxygen levels in the bloodstream (received through a nasal tube, face mask, or ventilator, depending on severity)
Prevention of Pneumonia
In many cases, it can be prevented.
-
Vaccination
The first line of defense is to get vaccinated. There are several vaccines that can help. Two vaccines help protect against pneumonia and meningitis caused by pneumococcal bacteria.
Prevnar 13 is effective against 13 types of pneumococcal bacteria. This vaccine is for: children under age 2, people between ages 2 and 64 with chronic conditions that increase their risk and adults ages 65 and older.
Pneumovax 23 is effective against 23 types of pneumococcal bacteria and is recommended for: adults ages 19-64 and people between ages 2 and 64 with chronic conditions that increase their risk.
Flu vaccine
Pneumonia can often be a complication of the flu, so it is important to be vaccinated against flu. And it is recommended for ages 6 months and above particularly those who may be at risk of flu complications.
Hib vaccine
This vaccine protects against Haemophilus influenza type b (Hib), a type of bacterium that can cause pneumonia and meningitis. The vaccine is recommended for:
- Under 5 years old.
- Unvaccinated older children or adults who have certain health conditions.
- People who’ve gotten a bone marrow transplant.
Please note that t if one is vaccinated, the symptoms may be mild and illness duration shorter as well as a lower risk of complications.
Pneumonia Complications
This illness may cause complications, especially in people with weakened immunityor chronic conditions medical conditions, such as DM.
Complications may include:
- Worsened chronic conditions. if you have certain preexisting health conditions, pneumonia could make them worse. E.g. Congestive
Heart failure, emphysema, Heart attack etc.
- Bacteremia. May spread to your bloodstream. This can lead to dangerously low blood pressure, septic shock and, in some cases, organ failure.
- Lung abscesses.
These are cavities in the lungs that contain pus. Antibiotics can treat them. Sometimes they may require drainage or surgery to remove the pus.
- Impaired breathing.
One may have trouble getting enough oxygen when breathingand there may be need to use a ventilator.
- Acute respiratory distress syndrome. This is a severe form of respiratory failure. It’s a medical emergency.
- Pleural effusion.
if pneumonia isn’t treated, one may develop fluid around the lungs in your pleura, called pleural effusion(the pleura are thin membranes that line the outside of your lungs and the inside of your rib cage). the fluid may become infected and need to be drained.
-
- Kidney, heart, and liver damage. These organs may be damaged if they don’t receive enough oxygen, or if there’s an overreaction of the immune system to the infection.
- Death.
Conclusion
Streptococcus pneumonia is still the most common pathogen in all age groups, settings, and geographic regions. However, the incidence of S. pneumonia infection has been declining because of increasing rates of vaccination and development of herd immunity.
However, pathogens of every sort, from viruses to parasites, can cause pneumonia. With the availability of sensitive molecular diagnostic methods, there is increasing recognition of viruses as a cause of pneumonia.
See a doctor right away if your symptoms get worse, as you may need to be hospitalized to prevent or treat more serious complications.