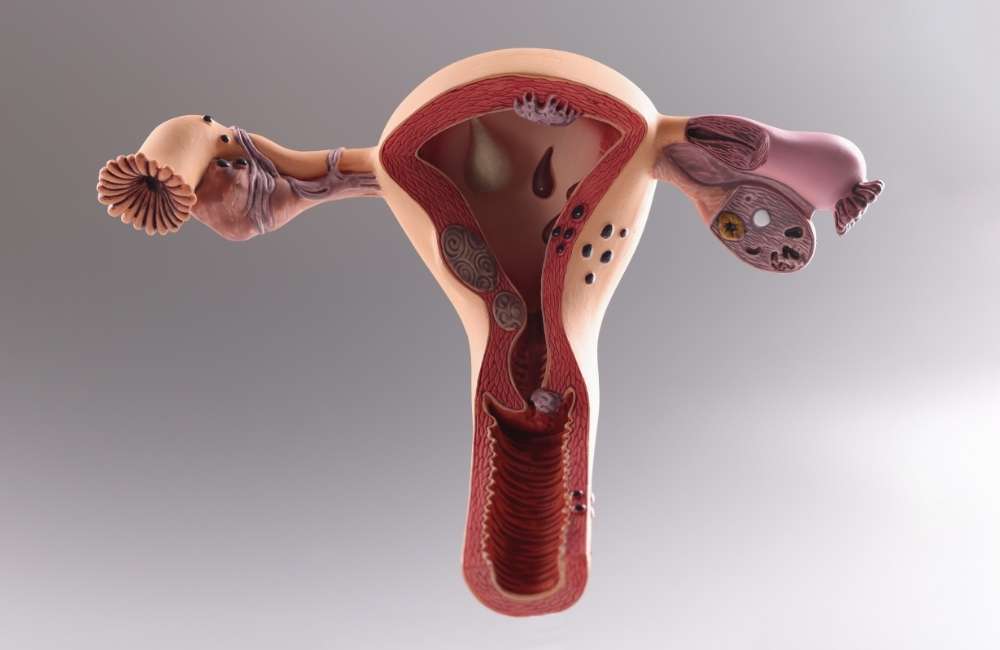
Pelvic inflammatory disease affects the uterus, fallopian tubes, and/or ovaries. It is typically an ascending infection, spreading from the lower genital tract. The female reproductive system /genital tract consists of two parts viz: the lower and upper genital tracts.
- The lower or external genital tract consists of:
-
- Mons pubis.
- Labia majora.
- Labia minora.
- Clitoris.
- Vestibule.
- Hymen.
- Bartholin’s glands.
- External urethra meatus, and skene’s gland.
- The upper or internal genitalia is the reproductive system and consists of:
-
- The vagina.
- Cervix.
- Uterus.
- Fallopian tubes.
- Ovaries.
Thus the inflammation of the upper or internal genital tract due to infection that usually ascends from the vagina and cervix to the uterine body, and fallopian tubes, and may spread to the ovaries resulting in Pelvic inflammatory disease (PID).
This is a common cause of morbidity and accounts for 1 in 60 GP consultations by women under the age of 45 years and de delays of only a few days in receiving appropriate treatment markedly increase the risk of sequelae, which include infertility, ectopic pregnancy and chronic pelvic pain.
What is a Pelvic Inflammatory Disease (PID)?
Pelvic inflammatory disease (PID) is defined as an inflammation of the upper genital tract that often stems from an untreated sexually transmitted infection or other gynaecological infections.
Causes of Pelvic Inflammatory Disease
In 85% of cases, sexually transmitted bacteria cause the infection. Of the offending agents, the bacteria Neisseria gonorrhoeae and Chlamydia trachomatis are the most common pathogens. Approximately 10% to 15% of women with endocervical N. gonorrhoea or C. trachomatis will go on to develop PID.
Typically, gonorrheal PID is more severe than PID due to other causes. PID due to chlamydia is less likely to cause symptoms, and therefore, more likely to result in subclinical PID. Subclinical PID can produce little to no symptoms but can still have adverse long-term consequences.
Other cervical microbes that cause the remaining 15% of cases are viz:
- Mycoplasma genitalium.
- Pathogens are responsible for bacterial vaginosis (Peptostreptococcus species, Bacteroides species).
- Respiratory pathogens (Haemophilus influenza, Streptococcus pneumonia, Staphylococcus aureus),
- Enteric pathogens (Escherichia coli, Bacteroides fragilis, group B Streptococci).
Risk Factors for Pelvic Inflammatory Disease

Apart from sexually transmitted infections, some factors increase the risk of developing PID viz:
- Childbirth, abortion or miscarriage
Bacteria that enter the vagina can spread more easily if the cervix is not fully closed.
- An intrauterine device (IUD)
A form of birth control that is placed into the uterus. This can increase the risk of infection, which may become PID.
- An endometrial biopsy
Procedure during which a sample of tissue is taken for analysis from the endometrium. This increases the risk of infection and subsequent PID.
- Appendicitis very slightly increases the risk, if the infection spreads from the appendix to the pelvis.
- A young and sexually active woman, having more than one sexual partner.
- Previous history of sexually transmitted infection, or pelvic inflammatory disease.
- Having a new sexual partner with chlamydia bacteria is common in young men, and it is asymptomatic in common.
- Retrograde menstruation
When blood flows backwards into the pelvis instead of out of the vagina during menstruation.
Symptoms of Pelvic Inflammatory Disease
The signs and symptoms of the pelvic inflammatory disease might be mild and difficult to recognize. Some women don’t have any signs or symptoms. When signs and symptoms of PID are present, they most often include:
- Pain — ranging from mild to severe — in your lower abdomen and pelvis
- Unusual or heavy vaginal discharge that may have an unpleasant odour.
- Unusual bleeding from the vagina, especially during or after sex, or between periods
- Pain during sex.
- Fever, sometimes with chills.
- Painful, frequent or difficult urination.
Investigations for Pelvic Inflammatory Disease
-
Blood Pregnancy Test
A pregnancy test should be performed on all women suspected of having PID to help exclude an ectopic pregnancy.
-
Endocervical Swab Microscopy, Culture and Sensitivity (ECS M/C/S) or Nucleic Acid Amplification Test (NAAT)
Testing for gonorrhoea and chlamydia should be done.
-
HIV Test
A viral screen should be done. Women who are HIV infected were previously thought to get clinically more severe PID but recent studies suggest that the differences may be minor and that they respond as well to treatment as patients who are not HIV infected.
-
VDRL
This rules out syphilis.
-
Pelvic Ultrasound with Doppler Interrogation
Diagnosis of pelvic inflammatory disease
The wide variation in symptoms and signs associated with PID can make diagnosis challenging. No single historical, physical, or laboratory finding is both sensitive and specific for the diagnosis of PID.

Clinicians should therefore maintain a low threshold for the diagnosis of PID, particularly in young, sexually active women.
- Pelvic examination to examine and check if there is tenderness or any other vaginal discharge especially green or yellow. Patients with PID will feel discomfort during examination when the cervix is excited.
- Laboratory examination: vaginal or cervical swabs, positive swaps will show antibodies for chlamydia or gonorrhoea that confirm the diagnosis of PID, on the other hand, a negative swap for chlamydia or gonorrhoea doesn’t rule out PID.
- Blood test: we will find an increase in white blood counts(WBC), C-Reactive proteins(C-RP), and Erythrocyte sedimentation rates(ESR) they support but they aren’t specific to PID and aren’t an accurate diagnosis.
- Ultrasound: the trans-vaginal ultrasound is used to exclude ectopic pregnancy, and ovarian swelling, findings may be normal.
- Laparoscopy is the gold standard to confirm PID diagnosis when the antibiotic course treatment fails.
Treatment for Pelvic Inflammatory Disease (PID)
If diagnosed at an early stage, PID can be treated with a course of antibiotics, which usually lasts for 14 days. A mixture of antibiotics to cover for the most likely infections is usually given.
Recent sexual partners also need to be tested and treated to stop the infection from coming back or being spread to others.
What are the Complications of PID?
Delayed treatment of PID has a strong association with worsened outcomes and long-term complications. However, even with timely treatment, long-term complications can occur. One study estimated that for females with PID between 20 to 24 years of age,
-
Chronic pain
Chronic pelvic pain is seen in as many as one-third of women with PID. The pain is thought to be related to inflammation, scarring, and adhesions from the infectious process. The strongest predictor of developing chronic pelvic pain related to PID is recurrent PID
-
Ectopic pregnancies
The increased risk for ectopic pregnancy following PID is also related to damage to the fallopian tubes. In one study, the rate of ectopic pregnancy following PID is approximately 7.8% while the non-PID ectopic rate is 1.3%.
-
Infertility
Infertility can also result from PID, regardless if the patient is symptomatic or asymptomatic from the pelvic infection. The infection can cause severe damage to the fallopian tubes, including loss of the ciliary epithelial cells of the fallopian tube and occlusion of the tube. Infertility related to PID is more likely to occur if chlamydia is the infectious cause, if there is a delay in treatment for PID, if the patient has recurrent episodes of PID, or if the case of PID is more severe.
-
A tubo-ovarian abscess (TOA)
A tubo-ovarian abscess (TOA) is a serious short-term complication of PID that is characterized by an inflammatory mass involving the fallopian tube, ovary, and, occasionally, other adjacent pelvic organs.
Conclusion
Pelvic inflammatory disease (PID) is an infection of the female reproductive system and it is often caused by sexually transmitted infection if left untreated can lead to infertility, ectopic pregnancy, chronic pain etc. so all women with suspected PID should see their GP or Gynecologist to have a pelvic examination to evaluate cervical discharge, cervical motion tenderness, uterine tenderness, adnexal tenderness, or masses at getting treated early.