Obstructive sleep apnea (OSA) is a very common type of sleep-related breathing disorder. During sleep, all of the muscles in the body relax; this includes the muscles that help keep the throat open so that air can flow into the lungs.
The throat is normally open enough during sleep to let air pass. In some people, however, the walls of the throat relax and narrow during sleep, interrupting normal breathing. This is called obstructive sleep apnea. (OSA).
Loud snoring (caused by air squeezing through the narrowed or blocked airway) is a telltale symptom of OSA, although not everyone who snores has sleep apnea.
What is Obstructive Sleep Apnea?
This is a sleep disorder characterized by repeated episodes of apnoea (airflow blockade for 10 seconds or more) and hypopnea (airflow reduction of greater than 50% for 10 seconds or more) throughout the night as a result of the complete or partial collapse of the airway with a resultant decrease in oxygen saturation.
Because, people with OSA may experience repeated episodes of apnea and hypopnoea throughout the night, this condition is sometimes also referred to as obstructive sleep apnea-hypopnoea syndrome (OSAHS).
It is also important to know that OSA is an extreme form of sleep-related upper airway resistance. Less severe forms of upper airway resistance that do not cause oxygen desaturation to include.
- Snoring.
- Upper airway airflow resistance causes noisy inspiration but without sleep arousal.
- Upper airway resistance syndrome is characterized by crescendo (gradually increasing) snoring terminated by respiratory effort-related arousals (RERAs).
Patients with upper airway resistance syndrome are typically younger and less obese than those with OSA and they complain of daytime sleepiness more than do patients with primary snoring. Frequent arousals occur, but strict criteria for apneas and hypopneas may not be present.
Symptoms, diagnostic evaluation, and treatment of snoring and upper airway resistance syndrome are otherwise the same as for obstructive sleep apnea.
Please note that obstructive sleep apnea (OSA) is different from central sleep apnea (CSA), which results when the brain fails to send signals to the breathing muscles during sleep due to instability in the respiratory control centre. Central sleep apnea is thus related to the function of the central nervous system. Also in Central sleep apnea, the airway is not blocked.
Causes of Obstructive Sleep Apnea
The causes of obstructive sleep apnea are often complex and a combination of factors viz genetic, health, and lifestyle factors have not been identified.

-
Genetic
Genes thought to be associated with the development of obstructive sleep apnea are involved in many body processes. These include communication between nerve cells, breathing regulation, control of inflammatory responses by the immune system, development of tissues in the head and face (craniofacial development), the sleep-wake cycle, and appetite control.
-
Health, and lifestyle factors
In adults, the most common cause of obstructive sleep apnea is excess weight and obesity, with associated enlargement of the soft tissue of the mouth and throat. Obesity accounts for about 60 to 70 per cent of individuals with OSA. It is thought that excess fatty tissue in the head and neck constrict airways and abdominal fat may prevent the chest and lungs from fully expanding and relaxing.
Risk Factors of Obstructive Sleep Apnea
Several risk factors come into play here viz:
- Anatomic risk factors (common among obese people).
-
- An oropharynx “crowded” by a short or retracted mandible
- A prominent tongue base or tonsils
- A rounded head shape and a short neck
- A neck circumference of more than 43 cm (more than 17 inches)
- Thick lateral pharyngeal walls.
- Lateral parapharyngeal fat pads.
- Postmenopausal status.
- Ageing.
- Alcohol or sedative use.
- A family history of obstructive sleep apnea
This is present in 25 to 40% of cases, perhaps reflective of heritable factors affecting ventilatory drive or craniofacial structure. The risk of OSA in a family member is proportional to the number of affected family members
What are the Symptoms of Obstructive Sleep Apnea?
Often the first signs of obstructive sleep Apnea are recognized not by the patient, but by the bed partner, friends or relations and teachers depending on the age of the patient.
Many of those affected have no sleep complaints. The most common signs and symptoms are viz:
- Excessive daytime sleepiness and fatigue.
- Snoring.
- Restlessness during sleep.
- Frequent nighttime awakenings/sudden awakening with a sensation of gasping for air or choking.
- Forgetfulness and difficulty concentrating.
- Headaches.
- Mood disturbances.
For children, the presentation may be somehow tricky and may include viz:
- Sluggishness or sleepiness is often misinterpreted as laziness in the classroom.
- Poor school performance.
- Unusual sleeping positions, such as sleeping on the hands and knees, or with the neck hyper-extended.
- Excessive sweating at night.
- Bedwetting.
Investigations for Obstructive Sleep Apnea
-
An Overnight Sleep Study
An overnight study is usually done and it is known as a polysomnogram (PSG). It is the gold standard test for the diagnosis of obstructive sleep apnea. This is performed in a sleep laboratory.
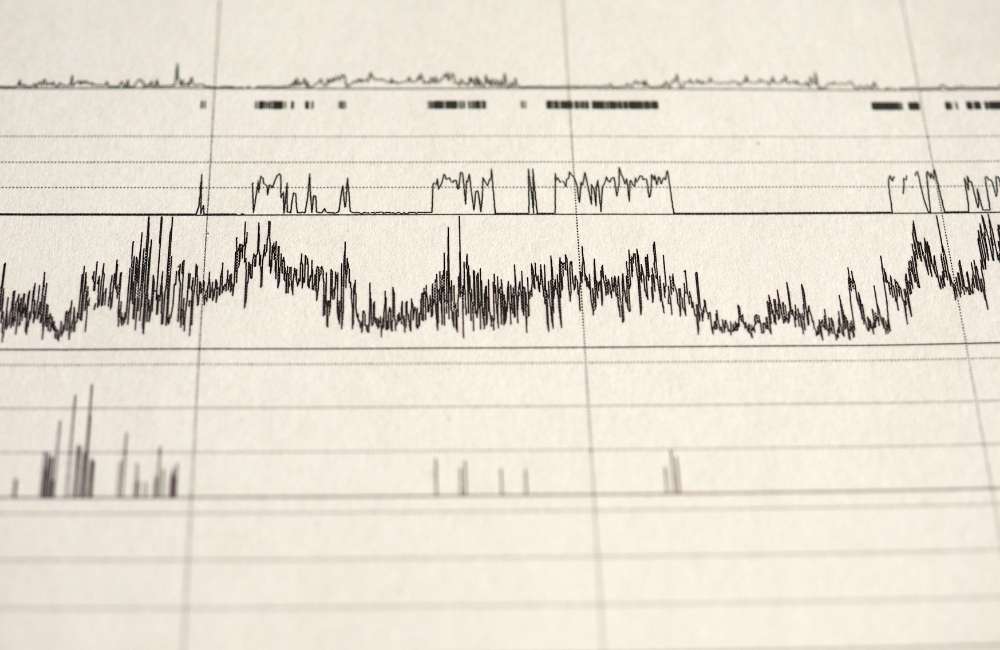
During the test, a variety of body functions, such as the electrical activity of the brain and the heart (EEG/EKG respectively), eye movements, muscle activity (EMG sensors), heart rate, breathing patterns, pressure sensors to detect nasal and oral airflow, and blood oxygen levels (pulse oximetry), temperature and respiratory impedance are recorded at night during sleep.
Also, plethysmography belts around the chest and abdomen detect motion. After the study is completed, the number of times breathing is impaired during sleep is tallied and the severity of the sleep apnea is graded.
-
Home Sleep Test (HST)
This is a modified type of sleep study that can be done in the comfort of a home. It records fewer body functions than PSG, including airflow, breathing effort, blood oxygen levels and snoring to confirm a diagnosis of moderate to severe obstructive sleep apnea.
Diagnosis of Obstructive Sleep Apnea
- Symptoms Criteria
- Sleep studies
The diagnosis of obstructive sleep apnea is suspected in patients with identifiable risk factors, symptoms, or both.
Criteria for diagnosis
These consist of viz.
- Daytime / Nighttime symptoms
-
- Daytime sleepiness.
- Unintentional sleep episodes.
- Unrefreshing sleep, fatigue, or difficulty staying asleep.
- Awakening with breath-holding, gasping or choking.
- Sleep monitoring that documents the following:
More than 5 episodes of hypopnea and/or apnea per hour with symptoms, or more than 15 episodes per hour in the absence of symptoms.
- Reports by a bed partner of loud snoring, breathing interruptions, or both in the patient’s sleep
Treatment of Obstructive Sleep Apnea
Treatment aims to normalize breathing during sleep and address any underlying health problems. The options will depend on the cause and severity of the symptoms.
-
Lifestyle Modifications and Control of Risk Factors
These are essential to normalizing breathing and are critical first steps in treatment viz:
-
- Heart Healthy Diet.
- Limiting the drinking of alcohol.
- Healthy sleeping Habits/sleeping more on the side.
- Stopping smoking.
- Weight reduction measures.
-
Continuous Positive Airway Pressure (CPAP) Therapy
This is the treatment of choice and the most effective treatment for sleep apnea. CPAP improves upper airway patency by applying positive pressure to the collapsible upper airway segment. Effective pressures typically range from 3 to 15 cm of water.
Disease severity does not correlate with pressure requirements. Many CPAP devices monitor CPAP efficacy and titrate pressures automatically, according to internal algorithms.
If clinical improvement is not apparent, CPAP efficacy should be reviewed and patients should be reassessed for a second sleep disorder (e.g., upper airway obstruction) or a comorbid disorder. If necessary, pressure can be titrated manually during monitoring
-
Mandibular Repositioning Device (MRD)
Here, an oral appliance, a mouthpiece is used in holding the jaw in a forward position during sleep thus expanding the space behind the tongue. This helps keep the upper airway open, preventing apnea and snoring.
Some problems using this device are jaw or tooth pain, and potential aggravation of the temporomandibular joint disease.
-
Adjunctive Treatments
-
- Pharmacotherapy
Several drugs have been tried (e.g. tricyclic antidepressants like theophylline etc.) but cannot be routinely advocated because of limited efficacy.
-
- Oxygen Administration
Supplemental oxygen improves blood oxygenation, but a beneficial clinical effect cannot be predicted. Also, oxygen may provoke respiratory acidosis and morning headaches in some patients.
-
Surgery
Surgery can be used in widening the airway in people with Obstructive sleep apnea or removing excess tissue or enlarged tonsils.
-
- Somnoplasty
Radiofrequency energy is used to tighten the tissue at the back of your throat.
-
- Uvulopalatopharyngoplasty (UPPP or UP3)
This procedure takes out soft tissue in the back (the uvula) and tissue from the soft palate of the throat, making the airway wider at the throat opening. Surgery is done in conjunction with a tonsillectomy and adenoidectomy.
-
- Nasal surgery
These operations correct obstructions in your nose, such as a deviated septum (when the wall between your nostrils is off-centre).
-
- Tracheostomy
It is the most effective therapeutic manoeuvre for OSA but is done as a last resort. It bypasses the site of obstruction and is indicated for patients most severely affected especially when OSA causes the left ventricle of the heart to enlarge or hypertrophy (cor-pulmunale).
Complications of Obstructive Sleep Apnea
Regularly interrupted or fragmented, non-restorative sleep has a big impact on the quality of life and thus increases the risk of personal safety, especially diving safety and developing certain medical conditions viz:
- Arrhythmias.
- Hypertension.
- Stroke.
- Heart attack.
- Type 2 DM.
- Mental illness.
- Sleepiness during the day and trouble concentrating. Adults may have a higher risk of accidents, and children may have a hard time at school.
Conclusion
Obstructive sleep apnea is the leading medical cause of excessive daytime sleepiness (aka wake-time sleepiness), increasing risks of automobile crashes, loss of employment, and sexual dysfunction. Relationships with bed partners and roommates and/or housemates may also be adversely affected because affected people may also have difficulty sleeping. So, if you notice these symptoms please report to your GP for proper assessment and treatment.

