Obesity is a global and complex public health concern associated with reduced life expectancy, a risk factor for a range of chronic diseases, viz (cardiovascular, liver, respiratory diseases, Diabetes (type 2) and some cancers)also obesity has a great impact on the mental health of the individual and this significantly affects their daily lives as well as increased mortality risks.
The economic burden of obesity is very high. Obesity is estimated to increase U.S. healthcare spending by $170 billion annually (including billions from Medicare and Medicaid).
Trust for America’s Health’s (TFAH) 19th annual report on the nation’s obesity crisis titled, ‘State of Obesity 2022: Better Policies for a Healthier America’ reported that four in ten American adults have obesity, and obesity rates continue to climb nationwide and within population groups.
It also stated that 19 states have an adult obesity rate of over 35 % with West Virginia, Kentucky, and Alabama having the highest rate of adult obesity at 40.6 per cent.
Whereas in the Uk, obesity statistics published Wednesday, 16 March 2022 has it that about 28% of adults in England are obese and a further 36% are overweight with male (68,2%)> female (60.4%) preponderance.
What is obesity?
Obesity is a chronic, complex, multifactorial, and largely preventable disorder that occurs when a person has such an excessive amount of body fat that they are at risk for adverse health conditions. Ultimately, obesity results from a long-standing imbalance between energy intake and energy expenditure, including energy utilization for basic metabolic processes and energy expenditure from physical activity.
Classification of Obesity: Am I obese?
In 1997, the World Health Organization International Obesity Task Force recommended the adoption of body mass index (BMI) as a standard for the assessment of body fat.
BMI is calculated by dividing a person’s weight in kilograms by one’s height in meters squared. Based on these guidelines, therefore:
- Normal BMI 18.5- 24.9 kg/m2.
- Overweight 25.0-29.9 kg/m2.
- Obesity ≥30 kg/m2.
Today, obesity along with being overweight has grown to epidemic proportions affecting over a third of the world’s population and if these secular trends continue, by 2030 it is speculated that an estimated 38% of the world’s adult population will be overweight and another 20% will be obese.
In Adults, obesity is classed based on BMI values- (weight/height2)
- Obese class 1 30.0-34.9kg/m2
- Obese class 11 35.0-39.9kg/m2
- Obese class 111 >40.0kg/m2
But in children, body weight classifications differ from those of adults because body composition varies greatly as a child develops, and further varies between boys and girls primarily owing to differences in sexual development and maturation therefore, childhood obesity can be diagnosed when a child’s BMI is at or above the 95th percentile of the sex-specific BMI-for-age growth charts. Being in the 95th percentile means that compared with other children of the same age and sex, the child has a higher BMI than 95% of them.
Obesity Causes
Causes of obesity are probably multifactorial and include the following:
-
Genetic predisposition
Genetics is now known to play a substantial role in the predisposition to obesity and may contribute to about 70% risk for the disease. Over 100 genes and gene variants discovered are related to excess weight yet genetic obesity risk does not always translate into actual obesity development, thus suggesting a complex interaction between genetics, behaviour and environmental influences. Therefore polygenic obesity is common in adults.
Genetic studies in the more common forms of obesity have also shown a region of chromosome 2 that influences obesity-related phenotypes in several different racial groups.
-
Endocrine disruptors (e.g. bisphenol A [BPA])
Early exposure to obesogens, a type of endocrine-disrupting chemical (eg, cigarette smoke, bisphenol A, air pollution, flame retardants, phthalates, and polychlorinated biphenyls) can alter metabolic set points through epigenetics or nuclear activation, increasing the propensity of developing obesity
-
Gut microbiome
Groundbreaking research in the last decade has emerged on the role of trillions of gut bacteria, the human microbiome in obesity, energy metabolism, and carbohydrate and lipid digestion thus opening promising therapeutic avenues for obesity.
The composition of the gut microbiome, early use of antibiotics and other factors that alter the composition of the gut microbiome may promote weight gain and obesity later in life.
Broad and sometimes dramatic changes in microbiome populations have been catalogued following gastric bypass surgery.
-
Sleep/wake cycles
Insufficient sleep (usually considered < 6 to 8 hours/night) can result in weight gain by changing the levels of satiety hormones that promote hunger.
-
Environmental factors
Migrant studies attest to the critical role of the environment in the development of obesity. A marked change in BMI is frequently observed when populations with a common genetic heritage live under new circumstances of plentiful food and little exercise.
-
Post pregnancy
About 15% of women permanently gain ≥ 20 lb with each pregnancy.
-
Drugs
The following drugs have been implicated in weight gain viz:
-
- Corticosteroids.
- Lithium.
- Traditional antidepressants (tricyclics, tetracyclic, monoamine oxidase inhibitors [MAOIs]).
- Benzodiazepines.
- Antiseizure drugs.
- Thiazolidinediones (e.g., rosiglitazone and pioglitazone.),
- Beta-blockers.
- Antipsychotic drugs.
-
Eating disorders
Two pathologic eating patterns may be associated with obesity:
-
- Binge eating disorder
This is also called compulsory overeating. People with binge eating disorder eat large amounts of food when they’re not hungry, eat food faster than other people do, and eat until they’re uncomfortable. Binge eating is associated with some cancers, heart disease, stroke, diabetes and other disorders. Obesity is usually severe, and large amounts of weight are frequently gained with pronounced psychologic disturbance.
-
- Night-eating syndrome (NES)
Night-eating syndrome (NES) is an eating disorder that occurs along with frequent sleep interruptions. People with NES feel like they won’t be able to get back to sleep without eating. They may wake up several times in one night to eat.
Untreated, NES makes it difficult to maintain a healthy weight. It also increases the risk of health problems like diabetes and high blood pressure.
Many people with NES also have depression or anxiety that is often worse at night.
-
Uncommon causes of weight gain
Uncommonly, weight gain is caused by one of the following disorders:
- Brain damage caused by a tumour (especially a craniopharyngioma).
- InfectionInfections particularly those affecting the hypothalamus.
This can stimulate the consumption of excess calories.
-
- Hyperinsulinism
This is excessive insulin production especially due to pancreatic tumours.
-
- Hypercortisolism
Here there is excessive cortisol production due to Cushing’s syndrome (which happens when there’s extra cortisol in the body. Cortisol, the “stress hormone,” is vital to regulating your blood sugar and turning food into energy). Unfortunately, too much of it caused by a medication or a tumour can cause weight gain, muscle weakness and more.
-
- Hypothyroidism
Hypothyroidism results when the thyroid gland fails to produce enough hormones, rarely a cause of substantial weight gain.
Diagnosis of Obesity
Obesity is diagnosed by the following methods viz:
-
Body mass index (BMI)
In adults, BMI is defined as the weight (kg) divided by the square of the height (m2). However, BMI is a crude screening tool and has limitations in many subpopulations. Some experts think that BMI cutoffs should vary based on ethnicity, sex, and age. Asians and many aboriginal populations have a lower cut-off (23 kg/m2) for being overweight. In addition, BMI may be high in muscular athletes, who lack excess body fat and may be normal or low in formerly overweight people who have lost muscle mass.
In children and adolescents, overweight is defined as BMI at the ≥ 95th percentile, based on the age and sex-specific growth charts.

-
Waist circumference
Another way to estimate the potential disease risk of obesity is to measure waist circumference.
Excessive abdominal fat may be serious because it places one at greater risk for developing obesity-related conditions, such as Type 2 Diabetes, high blood pressure, and coronary artery disease.
To correctly measure waist circumference:
- Stand and place a tape measure around your middle, just above your hipbones.
- Make sure the tape is horizontal around the waist.
- Keep the tape snug around the waist, but not compressing the skin
- Measure your waist just after you breathe out.
An increased waistline may be indicative of a higher risk of developing obesity-related conditions if:
- As a man, the waist circumference is more than 40 inches or
- A non-pregnant woman whose waist circumference is more than 35 inches.
-
Sometimes body composition analysis
Body composition—the percentage of body fat and muscle is also considered when obesity is diagnosed. Although probably unnecessary in routine clinical practice, body composition analysis can be helpful if clinicians question whether elevated BMI is due to muscle or excessive fat.
The percentage of body fat can be estimated by the following:
- Measuring skinfold thickness (usually over the triceps).
- Determining mid-upper arm muscle area.
- Bioelectrical impedance analysis (BIA)
This estimates the percentage of total body water directly and the percentage of body fat is derived indirectly.
BIA is most reliable in healthy people and in people with only a few chronic disorders that do not change the percentage of total body water (e.g., moderate obesity, diabetes mellitus).
- Underwater (hydrostatic) weighing.
This is the most accurate method for measuring the percentage of body fat. Costly and time-consuming, it is used more often in research than in clinical care. This measures the weight accurately while submerged.
-
- Imaging procedures, including CT, MRI, and dual-energy x-ray absorptiometry (DXA), can also be used to estimate the percentage and distribution of body fat but are usually used only for research.
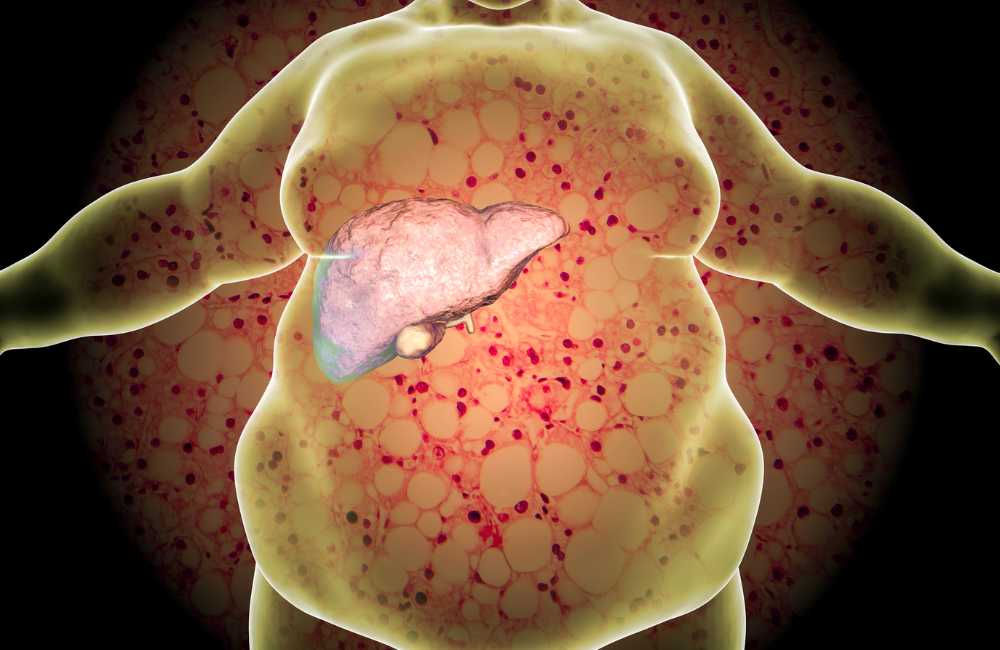
Complications of Obesity
- Diabetes.
- Cardiovascular diseases.
-
- Hypertension.
- Dyslipidemia.
- Coronary Heart Diseases.
- Heart failure.
- Stokes.
- Neurological problems
-
- Dementia.
- Alzheimer’s disease.
- Cancers
It is estimated that obesity accounts for about 20% of all cancer cases.
-
- Cancers of the colon, breast, endometrium, kidney and oesophagus.
- It is also associated with an increased risk of gastric, pancreatic and gallbladder cancers, as well as leukaemia.
- Respiratory complications
-
- Obstructive sleep apnoea
- Asthma
- Immune system complications
Obesity induces a deregulated immune system, which can be seen from childhood.
- Gastrointestinal complications
-
- Non-alcoholic fatty liver disease (NAFLD) is now the commonest cause of chronic liver disease worldwide. It is estimated to be present in 20–35% of adults in the developed world. One-third of these cases progress to non-alcoholic steatohepatitis (NASH), characterized by liver inflammation and injury, which can lead to cirrhosis and hepatocellular carcinoma.
- Gallbladder disease.
- Pancreatitis.
- Kidney disease
Being overweight and obese are risk factors for hypertension, diabetes, and other conditions associated with impaired renal function.
- Musculoskeletal system
-
- Gout
- Osteoarthritis (OA)
Obesity is associated with significant reductions in physical activity levels and is one of the main risk factors for osteoarthritis.
- Fertility
In men, obesity is associated with reduced sperm count and increased rates of erectile dysfunction. In women, it also leads to reduced fertility, poorer outcomes after fertility treatment and more pregnancy loss. Polycystic Ovarian Syndrome (PCOS) is the primary cause of female infertility and increases the rate of pregnancy complications.
- Psychosocial
Obese individuals are often exposed to public disapproval and stigma due to their weight, with women experiencing more discrimination. This takes place in employment, healthcare, education and other areas.
Depression is more common in obesity, particularly in women and younger people. Fat shaming leads to a lack of body image confidence, depression and suicidal thoughts.
Treatment of Obesity
There are several treatment options for obesity viz:
-
Dietary intervention
Diet control is the cornerstone of obesity management and its primary role should be emphasized to the patient. There are several dietary approaches to achieve this goal and please note that there is no miracle diet but eating a balanced diet with controlled portions is the best overall strategy.
-
- Low-calorie diet
Consisting of approximately 1000 to 1200 kcal/day. This has been successfully demonstrated to result in weight loss and decreases in abdominal fat.
-
- Very low-calorie diet
This only permits 400 to 500 kcal/day and has been found to promote initial weight loss between 13 and 23 kg. However, randomized controlled trials have shown that very low-calorie diets do not result in greater long-term weight loss when compared to low-calorie diets after1year.
-
- Changes in the dietary composition viz.
- Lower-fat diets promote weight loss by limiting the percentage of daily calories from fat to 20% to 30%.
- Low carbohydrate diet.
- Keto diet (High protein diet)-not a sustainable diet regimen.
- Mediterranean diet.-also confers cardiovascular benefits
- Dash diet. –Noted to decrease the blood pressure
-
Behavioural Therapy
Behavioural therapy refers to the application of psychological techniques to the treatment of obesity and is now an accepted modality of treatment.
Behavioural weight programs seek to alter lifestyle and environment to effect a weight change. They encourage the patient to become more aware of eating behaviour and physical activity and to focus on changing the behaviours that influence them.
The chief feature of this form of treatment is that it emphasizes personal responsibility for the initiation and maintenance of treatment.
Although the degree of weight loss achieved with behavioural techniques alone is modest, averaging less than 10 kg in most studies, the advantages include the lack of side effects and the low-attrition rate.
-
Exercises
Exercise alone results in only modest weight loss, studies consistently show the maintenance of weight loss for 2 years thus a combination of diet and exercise generally produces more weight loss than diet alone.
Regular exercise also results in a reduction in blood pressure, improvements in lipid profiles, glycemic control, and cardiovascular fitness.
-
Devices to reduce obesity
-
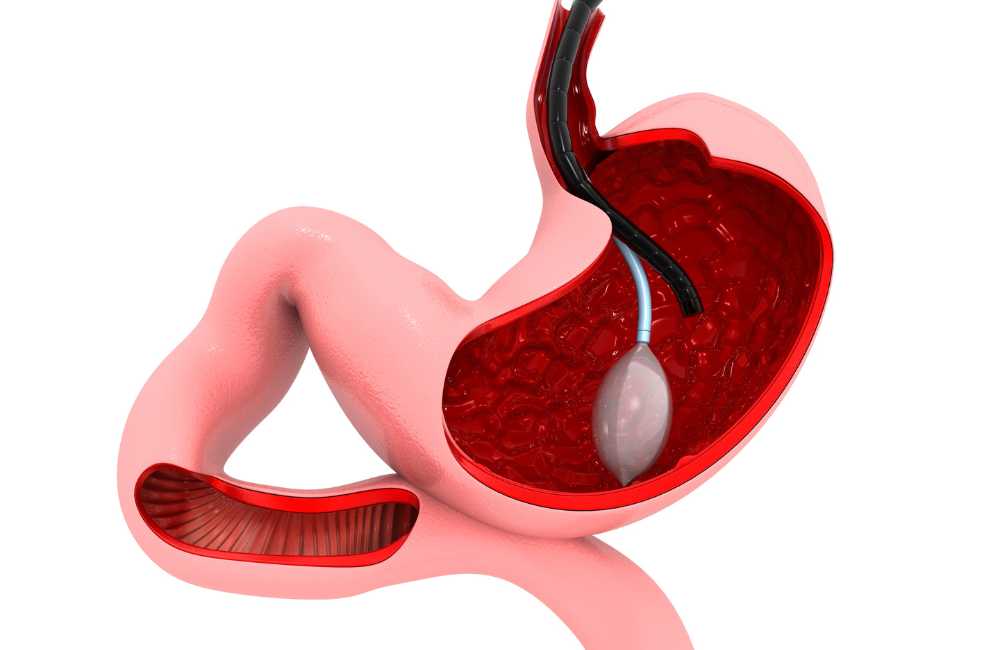
- Gastric balloons
The most modern gastric balloon is the adjustable Spatz weight loss balloon. This is endoscopically placed and kept in place for about 8 months. The Spatz 3 balloon can be downsized by deflating it when the gastrointestinal side effects become unbearable. A 15 % weight reduction has been reported with this device.
-
- Hydrogels
OralOral hydrogel therapy induces a feeling of fullness without adding calories for adults with overweight and obese. The product is ingested orally and creates small gel pieces that expand in the stomach making us the er feel full. It is taken with water twice a day before lunch and dinner.
-
Anti-obesity Medications – which one is the best?
Drugs used for obesity are a function of other co-morbidities like Diabetes type 2, depression/Anxiety, Headaches, binge eating etc. The following anti-obesity drugs are currently in use viz:
- GLP-1 agonist (Glucagon-like peptide 1).
This is a class of type 2 diabetes drugs that not only improves blood sugar control but may also lead to weight loss. E.g. Semaglutide (wegovy &Ozempic), liraglutide (Saxenda) and Trizepatide (Mounjaro). GLP-1 agonist can cause a 15 % weight reduction.
-
- Semaglutide
- Wegovy-Is specifically indicated for the treatment of overweight and obesity. Taken as a weekly injection and is available in 0.25 milligrams (mg), 0.5 mg, 1.0 mg, 1.7 mg and 2.4 mg pens.
- Ozempic- Ozempic is indicated for the treatment of Type 2 diabetes and is available in 0.25 mg, 0.5 mg and 1.0 mg pens.
- Rebels –This is the oral form of Semaglutide. FDA-approved for diabetes
-
- Liraglutide
- Saxenda (Liraglutide)-is a glucagon-like peptide-1 (GLP-1) receptor agonist that works by increasing feelings of being full and decreasing hunger in the brain and thus leading to eating fewer calories and losing weight. Usually taken once a week.
-
- Trizepatide (Mounjaro)
Trizepatide, sold under the brand name Mounjaro, is a medication approved by the FDA in May 2022 for the treatment of type 2 given by weekly injection under the skin and has been noted to cause about 22% weight loss (Not yet approved as an anti-obesity medicine). It’s the most effective weight loss medicine ever.
- Phentermine
Is a prescription medicine used to lessen appetite (Anorectics)? It can help weight loss by making you less hungry or can help you feel full longer.
Phentermine also is offered combined with topiramate for weight loss (Qsymia). The combined drug is approved for long-term use. Phentermine is approved for use for up to 12 weeks.
The combination can cause up to 8-10 % weight loss. But it isn’t a good choice for people with heart disease, high blood pressure, an overactive thyroid gland or glaucoma.
It also isn’t for people who are pregnant, planning to become pregnant or breastfeeding. Topiramate has issues with memory loss.
-
Surgery (Bariatric surgery)
Gastric bypass and other weight-loss surgeries — known collectively as bariatric surgery —involve making changes to your digestive system to help you lose weight. Bariatric surgery is done when diet and exercise haven’t worked or when you have serious health problems because of your weight.
This is a surgery to improve health. This isn’t a surgery to lose weight. For potentially life-threatening obese patients with type 2 Diabetes, a successful bariatric surgery means that their diabetes will be managed better, improves their chances of remission, reduces their need for diabetes medication and dramatically enhanced their quality of life.
Bariatric surgery new guidelines of eligibility.
- BMI of 35 and above irrespective of co-morbidities.
- BMI of 30-35 with co-morbidities.
- Asian individuals with a BMI of 27(Asians are considered obese at a BMI of 25 because they have a greater risk of DM etc. at a lower BMI.
- Barium surgery should be considered in children and adolescents who meet BMI criteria.
- No age limit to bariatric surgery.
Types of Bariatric surgery
- Roux-en-y gastric bypass
Is a type of gastric bypass that involves creating a small pouch from the stomach and connecting the newly created pouch directly to the small intestine.
- Endoscopic gastric bypass revision
This is also known as trans-oral outlet reduction surgery (ToRe). It is for patients who have regained weight following a previous surgical gastric bypass. Endoscopic suturing is used to reduce the size of the gastric pouch and the size of the outlet between the gastric pouch and intestine, helping patients to again lose weight.
- Endoscopic sleeve gastroplasty (ESG)
This is also known as the accordion procedure and it involves using an endoscope with an attached suturing device to place sutures in the stomach, this expands the top of the stomach thus making the stomach smaller and showing slowing stomach emptying with a feeling of fullness.
Recovery is 2-3 days with about 1-2% complications and between 17 to 21 % weight reductions.
- Laparoscopic sleeve gastrectomy (LSG)
Laparoscopic sleeve gastrectomy has become the most popular weight loss procedure in the United States over the last two decades. Long-term data is now available on the outcomes of sleeve gastrectomy, and it is very promising. The average excess weight loss after five years in a laparoscopic sleeve gastrectomy is reported to be around 60%, and the resolution of comorbidities is excellent.
Conclusion
Obesity is a chronic and relapsing condition with genetic, behavioural, socioeconomic, and environmental origins, fueled by economic growth, industrialization, mechanized transport, urbanization, an increasingly sedentary lifestyle, and a nutritional transition to processed foods and high-calorie diets.
Obesity greatly increases the risk of chronic disease morbidity—namely disability, depression, type 2 diabetes, cardiovascular disease, and certain cancers—and mortality.
There is no one size fits in the management of obesity. Seek advice and get the best treatment.