Jaundice is present in newborns due to the breakdown of red blood cells. At birth, newborns have a large number of red blood cells. Days after birth, the excess red cells are broken down with the released haemoglobin. The Heme molecules (from haemoglobin) are then converted to bilirubin, a yellow pigment.
There are 2 types of bilirubin viz:
- Unconjugated (indirect) Bilirubin.
- Conjugated (Direct) Bilirubin.
The majority of bilirubin produced from this breakdown of the red cell isin the unconjugated form. This binds to albumin in the blood and is transported to the liver where it is taken up by the liver cells and conjugated to make it water-soluble and excreted.
In adults conjugated bilirubin is further reduced by gut bacteria to urobilin and excreted in faeces but neonates, however, have fewer bacteria in their digestive tracts and so less bilirubin is reduced to urobilin and excreted. They also have an enzyme, which deconjugates bilirubin.
The now unconjugated bilirubin can be reabsorbed and recycled into circulation. This process is called the enterohepatic circulation of bilirubin. This process of converting the unconjugated bilirubin to a water-soluble, conjugated form sometimes overwhelms the newborn due to immaturity of their liver, this is worse with prematurity.
Failures of these processes result in the accumulation of excessive uncongested bilirubin thus leading to the Jaundice of the newborn. The good news is that in most cases, newborn jaundice goes away on its own as a baby’s liver develops and as the baby begins to feed, which helps bilirubin passes through the body.
What is Jaundice in Newborn Babies?
Jaundice is a yellow discolouration of the skin and eyes of the newborn child that occurs in 50-60 % of all newborns delivered at term in the first week of life and is caused by elevated serum bilirubin concentration.
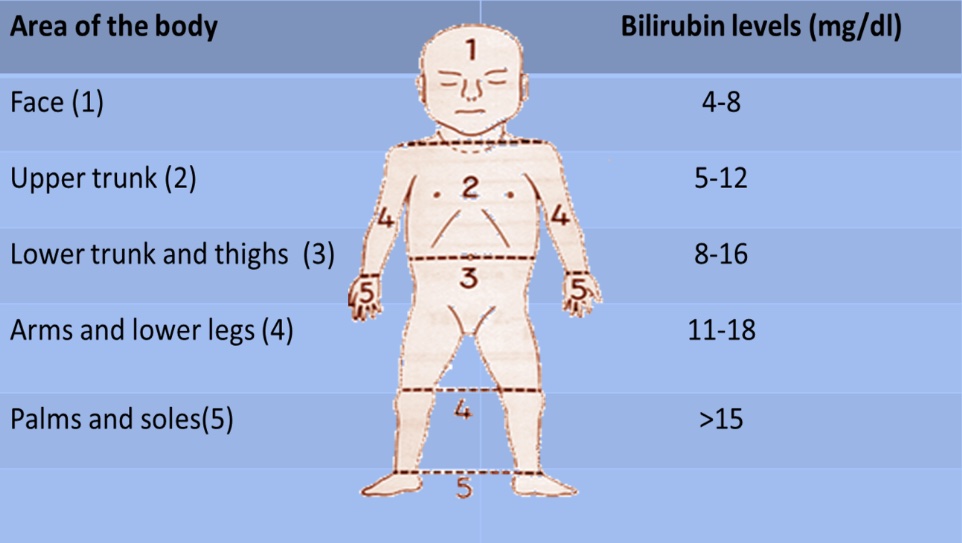
With increasing bilirubin levels, jaundice seems to advance in a head-to-foot direction, almost all the elevated serum bilirubin concentration in the immediate neonatal period is the unconjugated form.
The serum bilirubin level required to cause jaundice varies with skin tone and body region, but jaundice in the newborn usually becomes visible:
- On the sclera at about 2 to 3 mg/dL
- On the face at about 4 to 5 mg/dL
- The umbilicus at about 15 mg/dL
- The feet at about 20 mg/dL
Kramer’s scale indicates that neonatal jaundice begins from the newborn’s head; hence observation should be made from the face towards the feet as the level rises.
Why Worry About Jaundice?
This has been a source of anxiety and aggravation to families and doctors.
Elevated serum bilirubin may be harmless or harmful depending on its cause and the degree of elevation. Some causes of jaundice are intrinsically dangerous whatever the bilirubin level. But raised bilirubin of any aetiology is a concern once the level is high enough. The threshold for concern varies by:
- Age
Among healthy term infants, the threshold for concern typically is considered to be a level of more than 18 mg/dL.
- Degree of prematurity
Infants who are premature, and small for age are at greater risk and intervention may be done at lower levels. In such infants, risk increases with increasing serum bilirubin. The serum albumin concentration is also noted to be markedly low in preterm infants.
- Health status
- Sick infants with septicemias, low body temperatures and low oxygen levels in the body tissue are at great risk of developing Jaundice and intervention at lower bilirubin levels.
The major worry is neurotoxicity. This occurs when unconjugated bilirubin crosses the blood-brain- barrier and is deposited in basal ganglia and brain stem nuclei. This is followed by a variety of neurologic impairments, including cerebral palsy and kernicterus (the most severe form of neurotoxicity, although it is now rare still occurs and can nearly always be prevented.
Classifications
Raised serum bilirubin (hyperbilirubinemia) can be classified as:
- Physiologic or pathologic.
- Unconjugated or conjugated. (Biliary atresia (BA) is the most common cause of conjugated hyperbilirubinemia in infants).
- Classified by the mechanism of bilirubin production.
What Causes Newborn Jaundice?
-
Physiologic Jaundice
Occurs in almost all neonates. Can be a result of the following:
- Shorter red blood cell life span in newborns.
- Deficient conjugation is due to the deficiency of uridine diphosphate-glucuronosyltransferase (UGT), the enzyme responsible for conjugation.
- Low bacterial levels in the intestine combined with increased deconjugated of bilirubin lead to enterohepatic circulation.
-
Breast Milk Jaundice
Breast milk jaundice occurs late in the first week of life, peaks in the second, and usually resolves by two weeks of age. It is thought to be mainly due to inhibition of the UGT enzyme by pregnanediol and deconjugation of conjugated bilirubin in the intestines by beta-glucuronidase present in breast milk.
-
Breast Feeding Jaundice
Breastfeeding jaundice, also known as breastfeeding failure jaundice, occurs in the first week of life and is due to inadequate intake of breast milk leading to dehydration and sometimes very high sodium levels. Breastfeeding failure leads to decreased intestinal motility and decreases the elimination of bilirubin in the stool or meconium.
-
Blood group incompatibility
A baby whose blood type is incompatible with that of its mother can develop a buildup of antibodies that can destroy its red blood cells and cause a sudden rise in bilirubin levels.
-
Pathologic hyperbilirubinemia due to hemolytic disease
In term infants, this is diagnosed if:
- Jaundice appears in the first 24 hours or after the first week of life, or lasts for more than 2 weeks.
- Total serum bilirubin rises by more than 5 mg/dL/day.
- Total serum bilirubin is more than 18 mg/dL per day.
- An infant shows symptoms or signs of a serious illness.
Some of the most common pathologic causes are
- Immune.
- Non-immune hemolytic anaemia
- Non-immune causes include RBC enzyme defects, RBC membrane defects, hemoglobinopathies, sepsis, sequestration, and polycythemia.
- Hematoma resorption.
- Infections-Cytomegalovirus, HIV, rubella, herpes virus, syphilis, toxoplasmosis, urinary tract infection (UTI), septicemia.
- Low thyroid function.
Investigations for Jaundice
- Total Serum Bilirubin (TSB) and direct bilirubin levels.
- The blood type of both mother and baby.
- Direct coombs test to check for antibodies attached to the red cells.
- Complete blood count (CBC) with peripheral smear for red cell morphology.
Diagnosis of Jaundice
The evaluation of the neonate with jaundice starts with
- Detailed history.
- Birth history.
- Family history.
- The onset of jaundice.
- Maternal serologies.
- Colour of stool and urine.
- The presence of itching should be assessed for infants evaluated for jaundice and may provide a clue to the type of jaundice.
- Blood group incompatibility.
- A previous sibling who received phototherapy.

Assessment for jaundice
Assessment must be performed in a well-lit room or, preferably, in daylight or natural light at a window. It is first seen on the face and progresses caudally to the trunk and extremities as said earlier.
May sometimes appear and fade, blanching the skin with digital pressure on the forehead, mid-sternum or the knee/ankle to may reveal the underlying yellow colour of skin and subcutaneous tissue.
Diagnosis of raised serum bilirubin (hyperbilirubinemia) is suspected by the infant’s colour and is confirmed by measurement of serum bilirubin.
Noninvasive techniques for measuring bilirubin in infants, including transcutaneous and digital photography–based techniques, are being used increasingly and correlate well with serum bilirubin measurements. The risk of hyperbilirubinemia is based on age-specific total serum bilirubin levels.
Red flags
The following findings are of particular concern:
- Jaundice in the first day of life.
- Total serum bilirubin more than18 mg/dL.
- Rate of rising of total serum bilirubin by more than 0.2 mg/dL/hour or more than 5 mg/dL/day.
- Conjugated bilirubin concentration of more than 1 mg/dL if the total serum bilirubin is more than 5 mg/dL or more than 20% of total serum bilirubin (suggests neonatal cholestasis)
- Jaundice after 2 weeks of age.
- Lethargy, irritability, respiratory distress.
Jaundice Treatment
Treatment of hyperbilirubinemia is directed at the underlying disorder.
- Physiologic jaundice
Usually is not clinically significant and resolves within 1 week. Frequent formula feedings can reduce the incidence and severity of hyperbilirubinemia by increasing gastrointestinal motility and frequency of stools, thereby minimizing the enterohepatic circulation of bilirubin. The type of formula does not seem important in increasing bilirubin excretion.
- Breastfeeding jaundice
May be prevented or reduced by increasing the frequency of feedings. If the bilirubin level continues to increase for more than 18 mg/dL in a term infant with early breastfeeding jaundice, a temporary change from breast milk to formula may be appropriate; phototherapy
It also may be indicated at higher levels. Stopping breastfeeding is necessary for only 1 or 2 days, and the mother should be encouraged to continue expressing breast milk regularly so she can resume nursing as soon as the infant’s bilirubin level starts to decline. She also should be assured that the hyperbilirubinemia has not caused any harm and that she may safely resume breastfeeding. It is not advisable to supplement with water or dextrose because that may disrupt the mother’s production of milk.
Definitive treatment of hyperbilirubinemia involves
-
Phototherapy
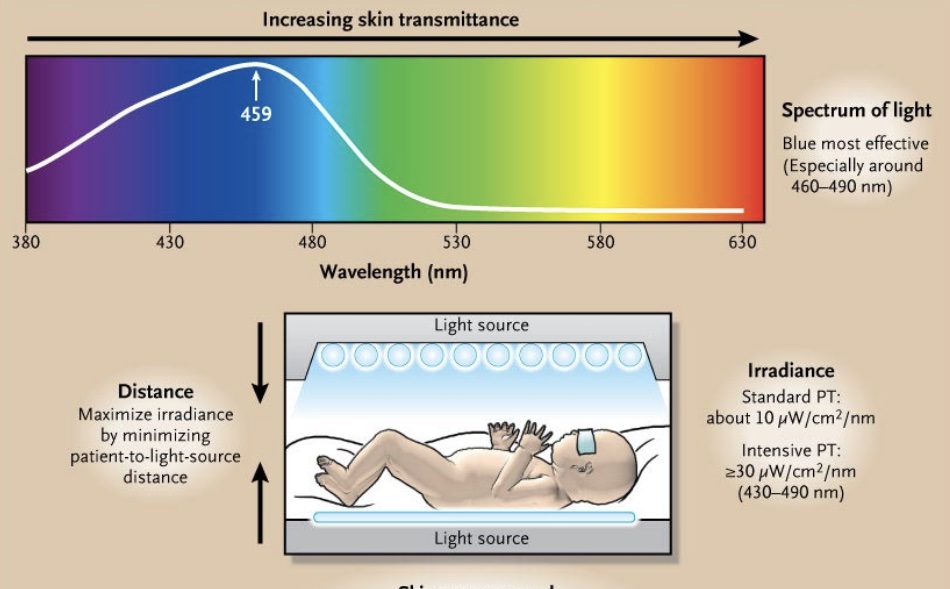
This treatment remains the standard of care, most commonly using fluorescent white light. Blue light, wavelength 460 to 490 nm, is most effective for intensive phototherapy. Phototherapy is the use of light to photoisomerize unconjugated bilirubin into forms that are more water-soluble and can be excreted rapidly by the liver and kidney without glucuronidation. It provides the definitive treatment of jaundice in newborns and prevention of kernicterus.
When To Stop Phototherapy
- Rate of decline variable, but a 6% to 20% decrease is expected
- In term infants without haemolysis, phototherapy can continue until the TSB level reaches 13 to 14 mg per dL.
- Infants do not need to be kept in the hospital to check for rebound hyperbilirubinemia, which is rare.
Care during Phototherapy
-
- Naked except for diapers.
- Eyeshields.
- The baby should be with a pulse oximeter.
- Keep watch on urine output.
- Daily weight monitoring
- Breastfeeding should be continued.
-
Exchange transfusion
This treatment can rapidly remove bilirubin from circulation and is indicated for severe hyperbilirubinemia, which most often occurs with immune-mediated hemolysis. Small amounts of blood are withdrawn and replaced through an umbilical vein catheter, or other access as available, to remove partially hemolyzed and antibody-coated red blood cells (RBCs) as well as circulating immunoglobulins.
The blood is replaced with uncoated donor RBCs that do not have the RBC membrane antigen that binds the circulating antibodies. That is, type O blood is used if the neonate is sensitized to AB antigens and Rh-negative blood is used if the neonate is sensitized to Rh antigen. Because adult donor RBCs have more ABO antigen sites than fetal cells, type-specific transfusion will intensify the hemolysis. Only unconjugated hyperbilirubinemia can cause kernicterus, so if conjugated bilirubin is elevated, the level of unconjugated rather than total bilirubin is used to determine the need for exchange transfusion.
Exchange transfusion is indicated in neonates with;
- Cord Hb 10 gm% or less.
- Cord bilirubin 5 mg% or more.
- Unconjugated serum bilirubin 10 mg% within 24 hours or 15 mg% within 48 hours or a rate of rising of 0.5 mg% per hour.
Complication
Newborns with very high bilirubin levels are at risk for bilirubin-induced neurologic dysfunction. This initially is reversible. However, if the condition progresses, patients can develop chronic bilirubin encephalopathy/kernicterus, which is then irreversible.
It manifests as cerebral palsy, seizures, arching, posturing, gaze abnormality, and sensor neural hearing loss. Patients are also at risk of developing liver failure, cirrhosis, and even hepatocellular carcinoma in a few cases.
Conclusion
Neonatal jaundice is a common condition with varied etiologies. Most cases are benign with an excellent prognosis and resolve with or without treatment. However, bilirubin encephalopathy can complicate clinical courses in a few.
Nurses and parents are often the first to notice jaundice in a newborn. After discharge from the birth hospital, parents need to be educated by the nurses, paediatricians, obstetricians, and family practice providers to monitor for jaundice and seek medical care if it worsens.

