Hydrocele is a painless swelling in the scrotum that occurs when fluid collects in the thin layer of skin surrounding a testicle called the tunica vaginalis (TV).
It usually occurs on one side but sometimes hydrocele forms in both testicles (testes). Little embryology and anatomy of the scrotum/the coverings of the testis may give us a proper understanding.
The scrotum is normally loose, soft and fleshy. It holds the two testicles (testes). Usually one can easily feel the testes in the scrotum.
The testes develop in the posterior abdomen in early fetal life and towards the end of pregnancy, they descend into the scrotal sac taking with it a blind-ended evagination of the abdominal wall that develops during fetal life called the processus vaginalis (also called the vaginal process).
This is an embryonic developmental outpouching of the peritoneum present from around the 12th week of gestation. In males, this precedes the testis in its journey through the abdominal wall down to the scrotum, and then fuses from a few weeks before birth, to a few weeks after birth.
The remaining portion of the processus vaginalis around the testes becomes the tunica vaginalis. So persistence of the processus vaginalis results in congenital hydrocele seen in babies.
In adults, the well-developed testes are covered by the tunica vaginalis which has two layers: one covering the testis, and the other reflected onto the scrotum, covering its inner surface thus creating a space between the two layers.
The tunica vaginalis secretes a trace quantity of lubricant into the space between its layers thus permitting free movement of the testes within the scrotum. Pathologically, if this space distends with fluid hydrocele develops in adult males.
What then is a hydrocele?
A hydrocele is an abnormal collection of serous fluid in a part of the processus vaginalis. This can occur in both male children and adult males. It is estimated that about 10% of newborn male infants have a hydrocele, which often clears up without any particular treatment within the first year of life.
In rare cases, similar fluid collections can develop in females along the canal of Nuck. (This results when there is a failed closure of the processus vaginalis in the female thus resulting in a continued outpouching of the parietal peritoneum through the inguinal canal to the labia majora.)
Types of hydrocele or ways hydroceles are described
Hydroceles are divided into two types viz primary and secondary.
-
Primary hydrocele
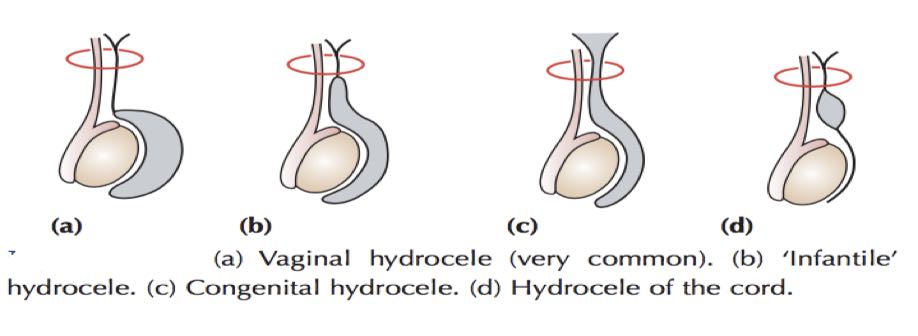
The processus vaginalis fuses at term or within 1-2 years of birth, thus obliterating the communication between the abdomen and scrotum. The distal portion, however, remains patent as the tunica vaginalis covers the testis, creating a potential space where fluid accumulation within it can lead to hydrocele formation. Depending upon the site of the obliteration of processus vaginalis, there are four types of primary hydrocele.
-
- Vaginal hydrocele
Processus vaginalis remains patent only around the testes and the fluid accumulation renders the testes impalpable.
-
- Infantile hydrocele
In this case, processus vaginalis gets obliterated at the level of the deep inguinal ring. However, the portion distal to it remains patent and allows fluid accumulation.
-
- Congenital hydrocele
This occurs when processus vaginalis is patent and communicates with the peritoneal cavity. This communication allows the movement of peritoneal fluid but is too small to allow the intra-abdominal contents to herniate through.
-
- Encysted hydrocele of the cord
Both the proximal and distal portions of processus vaginalis get obliterated while the central portion remains patent and fluid accumulates within it.
-
Secondary hydrocele
This usually occurs as a result of an underlying condition, such as:
-
- Infection (filariasis, tuberculosis of the epididymis, syphilis),
- Injury (trauma, hydrocele resulting after hernia repair),
- Malignancy.
This type of hydrocele tends to be small, except for secondary hydrocele due to filariasis, which can be very large.
What causes hydrocele?
There are four basic mechanisms by which hydrocele can develop viz:
- Connection with the peritoneal cavity (e.g congenital Hydrocele).
In children, patency of processus vaginalis allows the peritoneal fluid to flow in and out of the scrotum and this is the main cause of congenital hydrocele.
At birth, around 80-90% of term male infants have a patent processus vaginalis. This figure declines steadily to settle at approximately 25-40% at two years of age.
- Excessive production of fluid (secondary hydrocele).
- Defective absorption of fluid.
- Interference with the lymphatic drainage of scrotal structures (as in filarial hydrocele).
In adults, filariasis caused by Bucherer bancrofti is the main culprit globally, affecting more than 120 million people in more than 73 countries.
Filarial hydroceles account for up to 80% of hydroceles in tropical countries where the parasite Wucheria bancrofti is endemic. In this condition, the migration of the adult worms and then their presence in the scrotal lymph system result in hydrocele.
Chylocele may result from the rupture of the lymphatic vessels inside the scrotal cavity leading to (Lymphocele) or milky (Chyocele) fluid accumulation. Filarial hydroceles follow repeated attacks of filarial epididymal-orchitis.
They vary in size and may develop slowly or very rapidly. In longstanding chyloceles, there may be dense adhesions between the scrotum and its contents.
Filarial elephantiasis supervenes in a small number of cases. Treatment is by rest and aspiration. The more usual chronic cases are treated by excision of the sac.
- Trauma or post-hernia repair complications.
Post-herniorrhaphy hydrocele is a relatively uncommon complication of inguinal hernia repair.
In the United States, iatrogenic causes (either trauma or post-hernia repair complications) predominate.
Hydrocele symptoms
- Swollen scrotum
This is the most common symptom.
- Scrotal pain
Hydroceles usually don’t cause any pain. However, depending on the severity of the swelling, pain or discomfort may also occur.
- Heaviness in the scrotum
In adults, there may be a feeling of heaviness or a dragging sensation in the scrotum. In some cases, the swelling might be worse in the morning than in the evening.
For noncommunicating hydroceles, the size usually stays the same or grows very slowly.
- Hernia
With a communicating hydrocele, there’s the potential for other conditions to also develop. In this condition, fluid can travel in and out of the sac. But depending on the size of the remaining opening, it’s possible for a hernia to also develop.

Investigation
Laboratory tests are usually not indicated however; imaging studies (Scrotal Ultrasound scan & Duplex Ultrasonography) help diagnose and evaluate hydrocele. They can also assess for underlying processes such as epididymitis, testicular torsion, or testicular tumour and provide information regarding testicular blood flow, which will be reduced or absent in hydroceles resulting from testicular torsions.
Diagnosis of hydrocele
Diagnosis of Hydrocele is purely clinical. This is based on :
-
The history
The majority of patients with hydrocele present with complaints of painless scrotal swelling.
-
Clinical examinations
The examiner should look at this swelling in both the lying and standing positions. During the examination, the provider should ask the following set of three questions:
-
- Is it possible to reach above the swelling and palpate the cord? If not, this could represent a hydrocele (congenital or infantile) or a hernia. A hernia can be differentiated from a hydrocele in terms of having expansile cough impulse and reducibility but lacking transillumination (glow in light) and fluctuation.
- Does the swelling arise from the testis or epididymis or encase both of these structures? Hydroceles tend to surround both testes and epididymis, rendering them impalpable.
- Does the swelling transilluminate?
- Congenital hydrocele tends to be intermittent as it usually reduces when lying flat due to drainage of hydrocele fluid into the peritoneum. However, applying pressure on the congenital hydrocele does not reduce it.
- An encysted hydrocele feels like a smooth oval-shaped swelling near the spermatic cord. It may feel like an inguinal hernia and therefore, should be differentiated. In female patients, the hydrocele of the canal of the Nuck is a rare condition in which a cyst develops anterior to the round ligament of the uterus.
-
Results of imaging studies done
Hydrocele appears as an anechoic or echolucent area surrounding the testis( i.e. have a complete absence of echoes and therefore appears black on ultrasound image).
Can a hydrocele be prevented?
Unfortunately no, there are no known preventive steps to be taken to avoid hydroceles from developing in small babies, older children or adults. However, since injury is most often linked to hydroceles in teens and adults, taking precautions by wearing an athletic cup when in contact sports is a smart way to avoid developing a hydrocele.
Treatment of Hydrocele
-
Inactivity
Hydrocele in a newborn child may probably go away on its own in about a year. If this fails to resolve on its own or becomes very large, a need for surgery may be considered.
In adults, they might go away, especially if it was caused by inflammation like trauma or infection that has been treated. If they’re small, and exam and ultrasound results are promising, they’re usually monitored to see if they resolve on their own.
-
Needle aspiration
Hydroceles can also be treated by draining with a long needle. The needle is inserted into the sac fluid is drawn out. In some cases, a drug (sclerosant) may be injected to prevent the sac from filling again. Needle aspiration is commonly performed on those who are at high risk for complications during surgery.
Aspiration followed by an injection of a sclerosant (tetracycline or doxycycline) has been proven to be effective but painful. The most common side effects of needle aspiration are temporary pain and the risk of infection.
-
Sclerotherapy
Sclerotherapy is the injection of a solution to stop the hydrocele from recurring after having it drained. This is not commonly undertaken but may be offered to some people who are not suitable to have an operation.
-
Surgery
Surgery may be recommended if the hydrocele is large or uncomfortable. The operations for a hydrocele are of 2 types
-
- Hydrocelectomy
- Jaboulay’s procedure. The hydrocele sac is everted and anchored with sutures.
- Lord’s Procedure- the tunica is bunched into a ruff by applying a series of multiple interrupted chromic catgut sutures for the sac to form fibrous tissue.
-
- Herniotomy
Congenital hydroceles are treated by Herniotomy if they do not resolve.
This involves making a very small cut in the lower tummy (abdominal) wall. The passage between the abdomen and the scrotum will also be sealed off so the fluid cannot re-form in the future. This is a minor operation and is performed as a day case, so does not usually involve an overnight stay in the hospital.
Complications of Surgery
- Reactionary haemorrhage (Bleeding occurring within 24-48hrs after hydrocele surgery)
- Proceed (purulent collections within the tunica vaginalis)
- Infection.
- Sinus formation (Discharging blind-ended tract that extends from the surface of an organ to an underlying area or abscess cavity)
- Recurrent hydrocele.
Conclusion
Scrotal swelling can be alarming, but the cause is often benign. However, it is still best to consult a doctor as soon as possible to diagnose the cause of the swelling and recommend appropriate treatment options. This is because some causes of scrotal swelling can cause damage to the testicles and other important structures within the scrotum.

