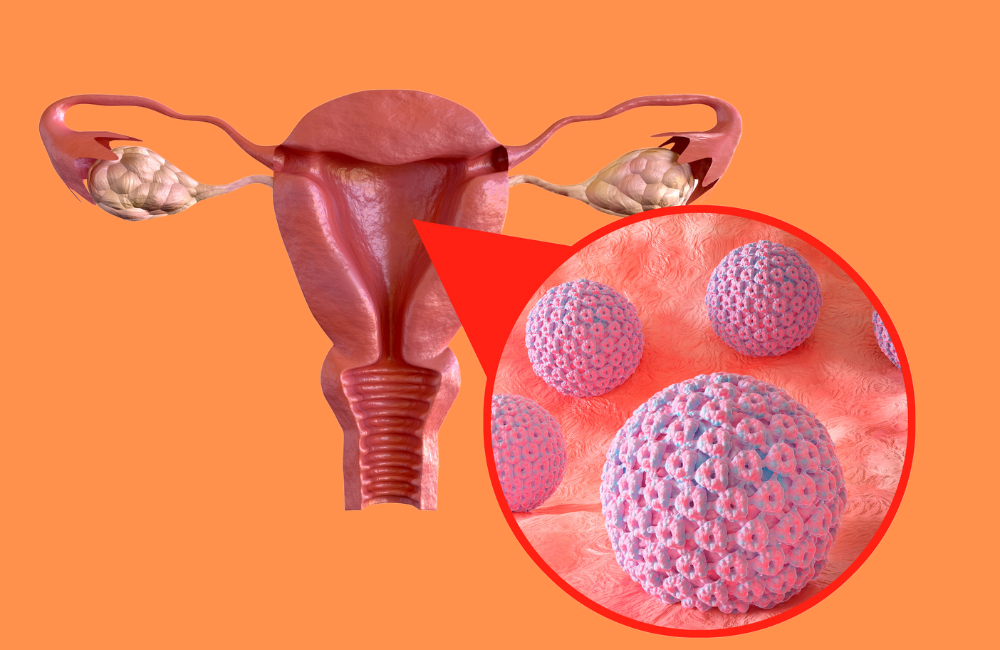
Human papillomavirus (HPV) infection is the most common sexually transmitted viral infection that’s passed between people through skin-to-skin contact.
Sexually transmitted infection with HPV is extremely common, with estimates of up to 75% of all women being exposed to HPV at some point in their life. However, almost all infected women will mount an effective immune response and clear the infection within 2 years without any long-term health consequences.
Persistent infection with human papillomavirus (HPV) is the principal cause of cervical cancer. The presence of HPV has been implicated in more than 99% of cervical cancers worldwide.
Both high-risk HPV genotypes (especially HPV-16 and 18), as well as persistent HPV infection (e.g. an infection that is not cleared by the patient’s immune system over time), are associated with an increased chance of progressing to high-grade cervical intraepithelial neoplasia (CIN) that is abnormal cells that are present on the surface of the cervix and invasive cancer.
HPV Causes
Human papillomaviruses (HPVs) are small non -enveloped, double-stranded DNA viruses that belong to the family of papillomavirus. About 170 HPV genotypes have been identified and approximately 40 kinds of these types, especially infect the anus and the genital areas.
Types of Human Papillomavirus
More than 170 HPV genotypes have been identified. Data suggest that certain HPV genotypes types (e.g. HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68) are considered high-risk (HR) for the development of cervical cancer.
Furthermore, HPV types 16 and 18 have been regarded as the genotypes most closely associated with the progression to cervical cancer. HPV-16 is the most carcinogenic and is associated with approximately 60% of all cervical cancers, while HPV-18 accounts for approximately 10% to 15% of cervical cancers.While6, 11, 42, 43, and 44 are regarded as low-risk HPV.
HPV Symptoms
Often, HPV infection doesn’t cause any noticeable symptoms or health problems. More than 90% of HPV cases will resolve spontaneously within 2 years but persistent infection can result in Genital warts, warts in the throat (also known as recurrent respiratory papillomatosis), cervical cancers and other cancers in the genitals and throat.

HPV can infect cells in the vagina and around the vulva. If a female has low-risk HPV, they may see warts on the vulva.
These warts may present as thus
- As clusters that look like cauliflower.
- As a scatter of bumps that are darker than unaffected skin.
- Growths that may be raised, flat, smooth, or rough.
In men with HPV infection penile or anal warts can be the presenting symptom.
Investigations for Human Papillomavirus
- Nucleic Acid (DNA) Testing by Polymerase Chain Reaction (PCR)
This has become a standard, non-invasive method for determining the presence of a cervical HPV infection. A positive result indicates the presence of human papillomavirus (HPV) DNA due to 1 or more of the following genotypes: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68.
Please, note that this test is not approved for use in men. A negative result indicates the absence of HPV DNA in the targeted genotypes.
- The Cobas Human Papillomavirus (HPV) Test
This is approved for cervical and endocervical samples. The Cobas HPV test detects DNA of the high-risk types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68. This test does not detect DNA of HPV low-risk types since these are not associated with cervical cancer and its precursor lesions.
Risk Factors for HPV
- Engaging in Unprotected sex (Vaginal, oral or anal sex).
- Multiple sexual Partners.
- Having a sexual partner that has HPV.
- A weakened immune system.
- Having other STIs, such as Herpes, Chlamydia and Gonorrhea.
Prevention of Human Papillomavirus
The best ways to prevent HPV are to use

- The use of barrier methods like Condoms (Male / female types).
- Safe sex.
- Vaccination.
The Gardasil 9 Vaccine is available for the prevention of genital warts and cancers caused by HPV. The vaccine can protect against nine types of HPV genotypes known to be associated with either cancer or genital warts.
The vaccine is recommended for boys and girls ages 11 or 12. Two doses of the vaccine are given at least six months apart. Women and men ages 15 to 26 can also get vaccinated on a three-dose schedule. Additionally, people between the ages of 27 and 45 who haven’t been previously vaccinated for HPV are now eligible for vaccination with Gardasil.
Treatment of Human Papillomavirus
Most HPV infections are self-limiting they resolve without treatment. There is no treatment for the virus itself. However, they are treatments for health problems caused by HPV.
Genital warts can be treated with prescription medications,
- Fulguration (Burning) with an electric machine called diathermy.
- Freezing with Liquid Nitrogen. Please note that getting rid of physical warts does not treat the virus itself, and warts may return.
- Cancers that develop from HPV may be treated by methods such as chemotherapy, or radiation surgery. Sometimes, multiple methods may be used.
Conclusion
Women aged 30 years and older with a negative Pap smear result but who are positive for HPV-16 and/or HPV-18, should consider referral for colposcopy if clinically indicated.
For women aged 30 years and older with a negative Pap smear, and positive-high risk -HPV test result, but who are negative for HPV-16 and HPV-18, consider repeat testing by both cytology and a high-risk -HPV test in 12 months. To prevent health problems associated with HPV, be sure to get regular health checkups, screenings, and Pap smears.