Hemorrhoids are enlarged veins in your bottom (anus). To understand this condition, it is good to know a little about the intestines. The large intestine is divided into 4 parts: The ascending, transverse and descending and the sigmoid colons.
The rectum is a chamber that begins at the end of the descending colon, immediately following the sigmoid colon, and ends at the anus. Ordinarily, the rectum is empty because stool is stored higher in the descending colon. When the descending colon becomes full, stool passes into the rectum thus causing an urge to move the bowels (defecate).
The anus is the opening where the gastrointestinal tract ends and exits the body. It starts at the bottom of the rectum. At the junction of the anus and the rectum is a sharp demarcation called the anorectal line or the dentate line?
This is a distinct anatomic landmark that divides the anal canal into two, upper and lower parts, although, this is not seen in clinical examination except when the patient is under anaesthesia.
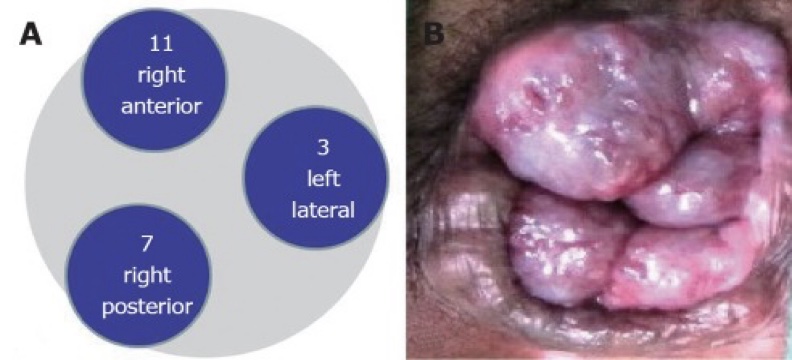
In the anal canal, there are areas of thickened anal mucosa, a condensation of hemorrhoidal vasculature called the anal cushions also called (Hemorrhoidal venous cushions) located at 11, 7 and 3 o’clock in the lithotomy position(the right anterior, right posterior, and left lateral zones).
They play an important role in maintaining continence by enabling tight closure of the rectum, because of their rich vascular supply, highly sensitive location, and tendency to engorge and prolapse, causing hemorrhoids. The hemorrhoidal venous cushions are common causes of anal pathology.
Confusion often arises because the term “hemorrhoid” has been used to refer to both normal anatomic structures and pathologic structures. In the context of this article, “hemorrhoids” refers to the pathologic presentation of hemorrhoidal venous cushions.
What are Hemorrhoids?
Hemorrhoids are a very common anorectal condition defined as the symptomatic enlargement and distal displacement of the normal anal cushions. They affect millions of people around the world and represent a major medical and socioeconomic problem.
Types of Hemorrhoids
The hemorrhoid classification system is useful not only to help in choosing between treatments but also to allow the comparison of therapeutic outcomes among them. Hemorrhoids are generally classified based on their location and degree of prolapse.
-
External hemorrhoids.
Are located below the dentate line and are covered by squamous epithelium.
-
Mixed Hemorrhoids.
Mixed (interno-external) hemorrhoids arise both above and below the dentate line.
-
Internal hemorrhoids.
Are located above the dentate line and are lined by rectal mucosa.
For practical purposes, internal hemorrhoids are further graded based on their appearance and degree of prolapse, known as Goligher’s classification:
- First-degree hemorrhoids (grade I): The anal cushions bleed but do not prolapse.
- Second-degree hemorrhoids (grade II): The anal cushions prolapse through the anus on straining but reduce spontaneously.
- Third-degree hemorrhoids (grade III): The anal cushions prolapse through the anus on straining or exertion and require manual replacement into the anal canal.
- Fourth-degree hemorrhoids (grade IV): The prolapse stays out at all times and is irreducible.
Acutely thrombosed, incarcerated internal hemorrhoids and incarcerated, thrombosed hemorrhoids involving circumferential rectal mucosal prolapse are also fourth-degree hemorrhoids.
Symptoms of Hemorrhoids
The most common manifestation of hemorrhoids is :
- Painless rectal bleeding associated with bowel movement is described by patients as blood drips into the toilet bowl. The blood is typically bright red.
- Prolapsing hemorrhoids may cause perineal irritation or anal itching due to mucous secretion or faecal soiling.
- A feeling of incomplete evacuation or rectal fullness is also reported in patients with large hemorrhoids.
- Pain is not usually caused by the hemorrhoids themselves unless thrombosis has occurred, particularly in external hemorrhoids or if a fourth-degree internal hemorrhoid becomes strangulated. Anal fissures and perianal abscesses are more common causes of anal pain in hemorrhoidal patients.
Hemorrhoids Diagnosis
The definite diagnosis of hemorrhoidal disease is based on:
- Precise patient history and careful clinical examination.
- Digital examination (DRE).
Although internal hemorrhoids cannot be palpated, the digital examination will detect an abnormal anorectal mass, anal stenosis, scar anal sphincter tone, and determine the status of prostatic hypertrophy, which may be the reason for straining that aggravates the descent of the anal cushions during micturition.
- Anoscopy in the left lateral position. The perianal area should be inspected for anal skin tags, external hemorrhoid, perianal dermatitis from anal discharge or faecal soiling, fistula-in-ano and anal fissure.
Hemorrhoidal size, location, the severity of inflammation and bleeding should be noted during anoscopy.

Risk Factors of Developing Hemorrhoids
- Constipation. Passing large stools and straining on the toilet increases the pressure in and around the veins in the anus and seem to be a common reason for piles to develop.
- A low-fibre diet.
- Being overweight. This increases your risk of developing piles.
- Pregnancy. Piles are common during pregnancy. This is probably due to the pressure effects of the baby lying above the rectum and anus, and also the effect that the change in hormones during pregnancy can have on the veins. Piles occurring during pregnancy often go away after the birth of the child.
- Ageing. The tissues in the lining of the anus may become less supportive as we become older.
- Hereditary factors. Some people may inherit weakness in the wall of the veins in the anal region.
- Heavy lifting or a persistent (chronic) cough.
Treatment of Hemmorhoids
Treatment of hemorrhoids ranges from dietary, lifestyle modification, and symptomatic treatment to radical surgery, depending on the degree and severity of symptoms
-
Dietary.
Increasing the intake of fibre or providing added bulk in the diet might help eliminate straining during defecation. In clinical studies of hemorrhoids, fibre supplement reduced the risk of persisting symptoms and bleeding by approximately 50% but did not improve the symptoms of prolapse, pain, and itching
Fibre supplement is therefore regarded as an effective treatment in non-prolapsing hemorrhoids; however, it could take up to 6 weeks for a significant improvement to manifest as fibre supplements are safe and cheap, and they remain an integral part of both initial treatment and a regimen following other therapeutic modalities of hemorrhoids.
-
Lifestyle modification
This should also be advised to any patients with any degree of hemorrhoids as a part of treatment and as a preventive measure. These changes include increasing the intake of dietary fibre and oral fluids, reducing consumption of fat, having regular exercise, improving anal hygiene, abstaining from straining and avoiding medication that causes constipation or diarrhoea.
-
Symptomatic treatment
Symptomatic treatment of hemorrhoids is usually all that is needed to get relief. It is accomplished by:
- Stool softeners (e.g., docusate, psyllium),
- WarmSitz baths (i.e., sitting in a tub of tolerably hot water for 10 minutes) after each bowel movement and as needed,
- Anaesthetic ointments containing lidocaine or witch hazel (hamamelis) compresses to soothe the site.
- Pain caused by a thrombosed external hemorrhoid can be treated with nonsteroidal anti-inflammatory drugs(NSAID)
-
Medical treatment
-
Oral flavonoids
They are capable of increasing vascular tone, reducing venous capacity, decreasing capillary permeability and facilitating lymphatic drainage as well as having anti-inflammatory effects.
-
Oral calcium dobesilate
This is another drug like the flavonoids commonly used in diabetic retinopathy and chronic venous insufficiency as well as in the treatment of acute symptoms of hemorrhoids. And is found to reduce tissue oedema. Calcium dobesilate, in conjunction with a fibre supplement, provided effective symptomatic relief from acute bleeding, and it was associated with a significant improvement in the inflammation of hemorrhoids.
-
Non Operative
-
Sclerotherapy
5% phenol in vegetable oil or other sclerosing agents can be used to treat bleeding internal hemorrhoids. Bleeding ceases at least temporarily.
-
Rubber band Binding
This is used for large, prolapsing/bleeding internal hemorrhoids or those that do not respond to conservative management. With mixed internal and external hemorrhoids, only the internal component should be rubber band ligated thus resulting in its necrosis and sloughing. Typically, one hemorrhoid is ligated every 2 weeks; 3 to 6 treatments may be required. Sometimes, multiple hemorrhoids can be ligated at a single visit, but this may cause more pain. External hemorrhoids should not be banded.
-
Infrared coagulation
Is useful for ablating non-prolapsing, bleeding internal hemorrhoids, or hemorrhoids that are not cured with rubber band ligation.
-
Radiofrequency ablation/Cryotherapy
Laser destruction, cryotherapy, and various types of electrodestruction are of unproven efficacy.
-
Operative treatment
-
Plication
Plication is capable of restoring anal cushions to their normal position without excision. This procedure involves over sewing of hemorrhoidal mass and tying a knot at the uppermost vascular pedicle. However, there are still several potential complications following this procedure such as bleeding and pelvic pain
-
Doppler-guided hemorrhoidal artery ligation
Hemorrhoidal artery ligation operation (known as HALO). During this procedure, arteries in your anal canal are closed to limit the blood supply to your piles. Sometimes an ultrasound probe will be used to help find your arteries and guide your surgeon during the procedure.
-
Hemorrhoidectomy
Surgical hemorrhoidectomy is required for patients who do not respond to other forms of therapy and for those who have grade IV internal hemorrhoids. Significant postoperative pain is common, as are urinary retention and constipation.
-
Stapled hemorrhoidopexy
Stapled hemorrhoidopexy is an alternative procedure for circumferential hemorrhoids and causes less postoperative pain but has higher recurrence and complication rates than conventional.
Prevention of Hemmorhoids

-
Eating plenty of fibre
(For example, fruit and vegetables, cereals, and wholegrain bread).
-
Taking lots of water
Ideally, water, although most sorts of drinks will do. Avoid too much alcohol, caffeine, and sugary drinks.
-
Taking fibre supplements
If a high-fibre diet is not helping to prevent constipation, you can take fibre supplements (bulking agents) such as Ispaghula, methylcellulose, bran or sterculia.
-
Avoiding certain painkillers
Some painkillers contain codeine such as co-codamol. They are a common cause of constipation. However, simple painkillers such as paracetamol may help.
-
Toileting
Go to the toilet as soon as possible after feeling the need (don’t hold it in). Equally, do not strain on the toilet.
-
Getting regular exercise
This helps to reduce constipation.
Hemmorhoids Complications
- Anaemia.
- Blood clots in external hemorrhoids(Thrombosis)
- Infection.
- Skin tags (flap of tissue that hangs off skin).
- Strangulated hemorrhoids (muscles in the anus cut off blood flow to a prolapsed internal hemorrhoid).
Conclusion
Treatment of hemorrhoids ranges from dietary, lifestyle modification, and symptomatic treatment to radical surgery depending on the degree and severity of symptoms. Although surgery is an effective treatment for hemorrhoids, it is reserved for advanced diseases and it can be associated with appreciable complications.

