Glaucoma is a leading cause of reversible blindness, often called the ‘silent blinder’ because there are no noticeable symptoms in the early stages; so early detection and treatment are key to preventing vision loss.
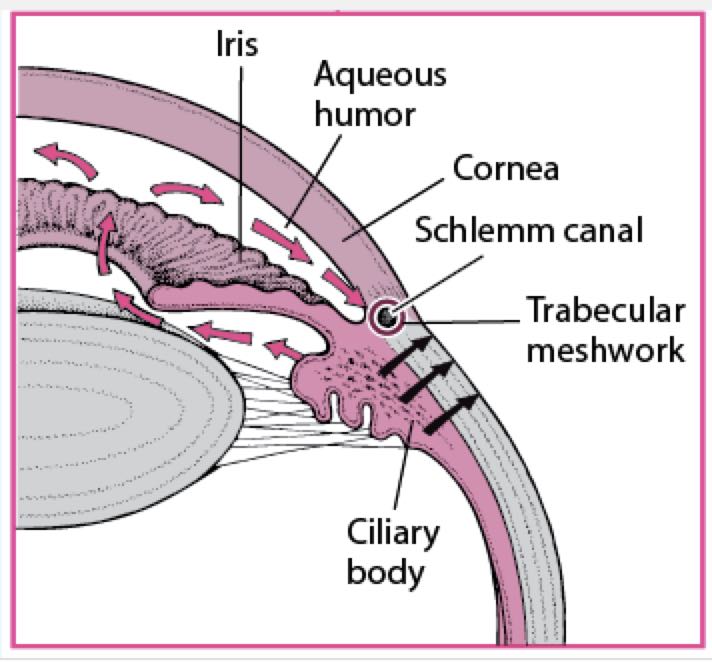
Little knowledge of the anatomy of the eye will help elucidate what happens in Glaucoma. There is a pressure build-up in the eyes leading to damage to the optic nerves.
Anatomy of the Eye
The Ciliary bodies produce the aqueous humour – which fills the anterior and posterior chambers of the eye. It is one of the fundamental components in ensuring that the optical physics and health of your eye are properly maintained.
Continuous production of aqueous humour is critical to the eye’s shape and size, and the quality of the image it produces. The aqueous humour thus has the following functions viz:
- Transports vitamin C in the front segment to act as an antioxidant agent.
- Provides inflation for expansion of the cornea (increasing protection against dust, grains, wind, pollen and several pathogens).
- Maintains intraocular pressure.
The produced aqueous humour exits the eye between the angle formed by the iris and the cornea via the trabecular meshwork and the scheme canal (see the diagram below) although a little quantity of aqueous humour is drained via the Ciliary body (aka the uveoscleral pathway).
In early adulthood, the ratio of drainage is approximately equal in both pathways but with ageing, drainage is predominate via the trabecular meshwork and the scheme canal.
Also, it’s good to note that branches of the optic nerve, that control the eye carry visual information from the eye to the brain, thus damage to these branches causes ganglion death and resultant optic nerve atrophy and patchy vision loss and it is known that elevated intraocular pressure plays a role in this damage either by direct nerve compression or reduced blood flow.
Normal intraocular pressure (IOP) is between 11 -21mmHg-This is maintained by the balance between the aqueous humour production and drainage.
If the IOP is more than 21 mmHg, ocular Hypertension is said to develop. Although some groups of patients with Glaucoma have a normal IOP. They are referred to low or normal tension Glaucoma.
What is Glaucoma?
Glaucomas are a group of eye disorders characterized by progressive optic nerve damage in which an important part is a relative increase in the intra-ocular pressure that can lead to an irreversible loss of vision.
Types of Glaucoma
- Open-Angle Glaucoma
The most common form of glaucoma, this type is caused by damage to the filter in the eye’s drainage canals.
- Angle-Closure Glaucoma
This type of glaucoma is caused by a rapid blockage of the eye’s drainage canals due to a closed or narrow-angle between the iris and cornea where the filter is located.
- Low-Tension or Normal-Tension Glaucoma
A type of glaucoma in which damage occurs to the optic nerve without eye pressure exceeding its normal range.
- Congenital Glaucoma
A type of glaucoma that occurs in infants when there are incorrect or underdeveloped drainage canals in the eye during the prenatal period.
- Uveitic (inflammatory) Glaucoma
This type of glaucoma is caused by autoimmune and inflammatory disorders.
- Neovascular Glaucoma
A type of glaucoma associated with poorly controlled diabetes and other conditions that damage the blood vessels in the body.
- Pigmentary Glaucoma
In pigmentary glaucoma, small pigment granules flake off from the iris and block or slow fluid drainage from the eye.
Risk factors / Causes of Glaucoma
Many factors lead to glaucoma. While increased ocular pressure (IOP)is the only modifiable risk factor known at this time, it is not a cause. It can also develop with normal eye pressure and can damage vision before any symptoms are noticed. So be aware of these risk factors viz:
- Increased intraocular pressure (IOP).
- Age over 55.
- Black, Asian or Hispanic heritage.
- Family history of glaucoma.
- Certain medical conditions, such as diabetes, migraines, high blood pressure and sickle cell anaemia.
- Corneas that are thin in the centre.
- Extreme nearsightedness or farsightedness.
- Eye injury or certain types of eye surgery.
- Taking corticosteroid medicines, especially eye drops, for a long time.

What are the Symptoms of Glaucoma?
- No Symptoms – Most people with glaucoma do not notice symptoms until they begin to lose their eyesight.
- Blurred or narrowed field of vision.
- Severe pain in the eyes.
- Seeing halos or “rainbows” around lights.
- Nausea/Vomiting.
- Headache.
Investigations for Glaucoma
The following eye investigations or tests should be done viz:
- Visual acuity test (VA)
This test measures how well you can see at various distances.
- Pupil dilation
Here, the pupil is widened with eye drops to allow a close-up exam of the eye’s optic nerve and retina.
- Visual field
This test measures a person’s side or peripheral vision. Lost peripheral vision may mean a person has glaucoma.
- Tonometry
This measures the ocular pressure(OP) of the eye.
- Optic nerve imaging
Photographs of the optic nerve are taken to indicate areas of damage.
- Gonioscopy
A lens is placed on the eye to look at the area called the drainage angle. This is where fluid drains from the eye. This test determines whether the drain is open or closed and if any damage has occurred.
- Tachymetry
This measures the corneal thickness.
How is Glaucoma Diagnosed?
A diagnosis can be scary. Many older people are dealing with several problems that come with age. They often worry that they will become a burden to the family if they lose their vision.
Reassure your patients that many people keep their vision with proper medication and care. The diagnosis is based on the history, clinical examination and the results of the above-mentioned investigations.
Treatment of Glaucoma
Patients with characteristic optic nerve and corresponding visual field changes are treated regardless of whether there is increased ocular pressure (IOP). Lowering the IOP is the only clinically proven treatment.
Two methods are available but the type of glaucoma determines the appropriate method to be used viz:
-
Drugs
Some medicines cause the eye to make less fluid, while others lower pressure by helping fluid drain from the eye. Prophylactic IOP lowering in patients with ocular hypertension delays the onset of glaucoma.
However, because the rate of conversion from ocular hypertension to glaucoma in untreated people is low, the decision to treat prophylactically should be individualized based on the presence of risk factors, the magnitude of IOP elevation, and patient factors (i.e. preference for drugs vs. surgery).

Generally, treatment is recommended for patients with IOP > 30 mm Hg even if the visual field is full and the optic nerve disk appears healthy because the likelihood of damage is significant at that IOP level.
-
Surgery
- Laser surgery
Several types of surgery using a laser are used to treat glaucoma.
-
- Trabeculoplasty. This opens the drainage area.
- Iridotomy. This makes a tiny hole in your iris to let fluid flow more freely.
- Cyclophotocoagulation. This treats areas of the middle layer of your eye to lower fluid production.
- Cataract surgery
Cataract surgery has been shown to reduce eye pressure in most cataract patients, and in some situations, it may be used as a treatment for glaucoma.
- Incisional surgery
Traditional incisional surgeries (e.g., guarded filtration procedures [trabeculectomy], glaucoma drainage implant devices [tube shunts]) create a new drainage pathway between the anterior chamber and subconjunctival space. Newer incisional surgeries enhance trabecular or uveoscleral outflow without creating a full-thickness fistula.
- Minimally invasive glaucoma surgeries (MIGS)
This is a newer, less invasive form of surgery, which usually requires tiny openings and uses devices you can’t see with the naked eye. It’s generally faster and safer but won’t lower pressure by quite as much.
Preventing Glaucoma
Regular eye examinations are recommended. Regular comprehensive eye exams can help detect glaucoma in its early stages before significant damage occurs. A comprehensive eye exam is recommended as follows viz:
- Every 5 to 10 years if you’re under 40 years old.
- Every 2 to 4 years if you’re 40 to 54 years old.
- Every 1 to 3 years if you’re 55 to 64 years old.
- Every 1 to 2 years if you’re older than 65.
If you’re at risk, you’ll need more frequent screening, checking the visual fields with frequency-doubling technology (FDT) perimetry and ophthalmoscopic evaluation of the optic nerve.
Although IOP should be measured, screening based only on IOP has low sensitivity, low specificity, and low positive predictive value. Ask your healthcare provider to recommend the right screening schedule for you.
Conclusion
Glaucoma is very common. It sometimes comes without symptoms, so early detection and treatment can save your vision.

