Gastro oesophageal reflux disease (GORD) is a condition whereby acid from the stomach leaks into the oesophagus. Let’s look at the anatomy of the oesophagus and how swallowing happens in a healthy patient.
The oesophagus is a 25cm hollow, muscular tube whose main function is to transfer food from the mouth to the stomach in a coordinated fashion. At the opening of the upper oesophagus, is a ring-shaped muscle called the upper oesophagal sphincter (UES).
This sphincter is normally closed at rest and serves as a protective mechanism against the regurgitation of oesophagal contents into the respiratory passages. It also serves to stop air entering the oesophagus other than the small amount that enters during swallowing.
Once the food is inside the oesophagus, waves of muscular contractions, called peristalsis, push it down through the diaphragm to reach the lower oesophagus.
At the opening of the lower oesophagus, there’s another ring-shaped muscle, called the lower oesophagal sphincter (LES). Like the upper oesophagal sphincter (UES) which opens in response to a primary peristaltic wave, the sphincter also relaxes to allow air to escape from the stomach at the time of vomiting.
A variety of factors influence sphincter tone, notably food, gastric distension, gastrointestinal hormones, drugs and smoking.
It usually stays shut to prevent stomach acid and digestive juices from getting into your oesophagus. Thus a normal, healthy valve serves as an effective anti-reflux barrier and experts consider it the most important factor in preventing GORD.
For people with GORD, this valve becomes dysfunctional and does not close appropriately and thus allowing abnormal amounts of both acidic and non-acidic fluids to backwash or reflux into the oesophagus.
What is Gastro Oesophageal Reflux Disease (GORD)?
Gastro oesophageal reflux disease (GORD) is a chronic gastrointestinal disorder characterized by the regurgitation of gastric contents into the oesophagus
Causes of Gastro Oesophageal Reflux Disease
Currently, there is no known cause to explain the development of the GORD. Over the years, several risk factors have been identified and implicated in the pathogenesis of GORD and they can be classed into Viz:
-
Motor Abnormalities
- Impaired Lower Oesophagal Sphincter (LES) Resting Tone
The LES is an anatomically complex zone located at the gastro-oesophagal junction, comprising two components: the true LES, a segment of tonically contracted smooth muscle located in the distal oesophagus and the crural portion of the diaphragm.
Both the LES and the diaphragm contribute to gastro-oesophageal sphincter competence. Physiologically, relaxations of the LES, before contractions of the oesophagus, allowing food to pass through into the stomach.
In resting conditions, LES maintains a high-pressure zone that is 15-30 mmHg above intragastric pressures (pressure in the stomach) depending on individual variability.
Some patients with GORD have a constantly weak, low-pressure LES, which permits reflux every time the pressure in the stomach exceeds the LES pressure. This occurs when LES pressure is less than 6 mmHg.
A chronically decreased LES resting tone is usually associated with severe esophagitis. Similarly, LES defects have been found in many patients with other GORD complications, such as oesophageal stricture and Barrett’s oesophagus.
Factors that decrease LES tone include:
-
- Endogenous hormones (cholecystokinin).
- Progesterone in pregnancy.
- Medications (nitrates, calcium channel blockers, etc.).
- Specific foods like high-fat meals and chocolate.
- Habits like smoking, caffeine and alcohol.
- Transient LES relaxations (TLESR)
TLESRs are brief episodes of LES relaxation unrelated to swallowing or peristalsis.
TLESRs account for 48-73% of reflux episodes thus TLESRs account for the majority of gastro-oesophageal reflux episodes.
Patients with GORD have an equal frequency of TLESRs compared with normal individuals, although they have a higher percentage of TLESRs associated with reflux.
- Impaired oesophageal acid clearance
Indeed, the process of oesophagal acid clearance is an important protective mechanism against GORD development. This process involves peristalsis as well as the swallowing of salivary bicarbonate.
Both primary and secondary peristalses are essential mechanisms of oesophagal clearance.
Swallowing-related primary peristalsis occurs about 60 times per hour, while secondary peristalsis occurs in the absence of swallowing and can be elicited by oesophagal distension or acidification. The swallowing of saliva (pH 7.8-8.0) is crucial in the completion of oesophagal acid clearance and restoration of oesophagal ph.
- Delayed gastric emptying
A delay in gastric emptying results in the extended retention of acidified gastric contents in the stomach during the post-prandial period, which may increase the likelihood of GORD.
-
Anatomical factors
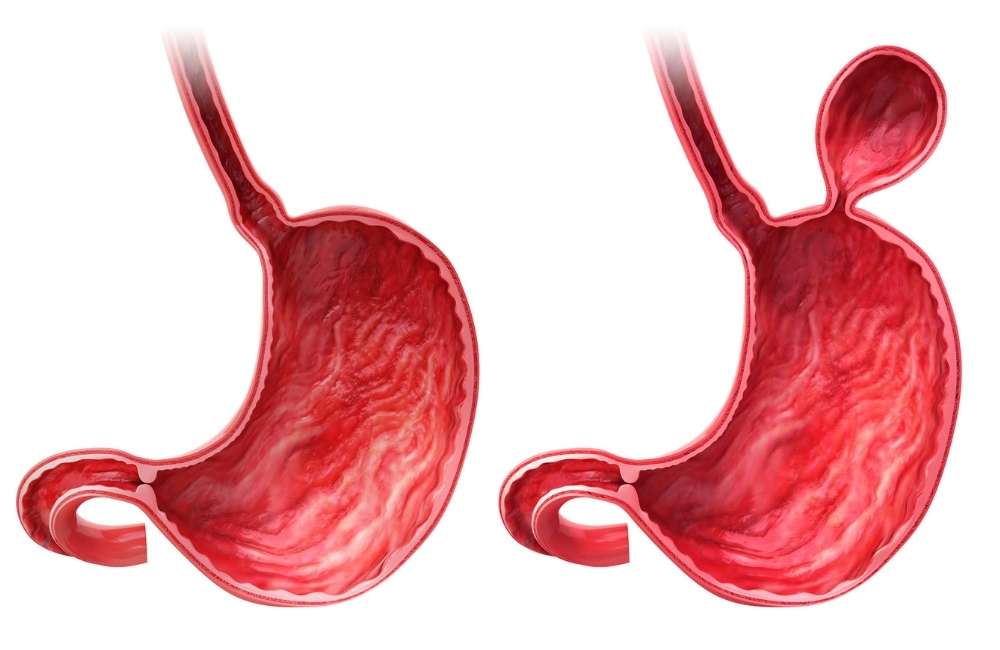
- Hiatal hernia
Some, but not all people with hiatal hernia have GORD and vice versa. A hiatal hernia occurs when a part of the stomach moves above the diaphragm. The diaphragm is a muscle that separates the chest (containing the oesophagus) from the abdomen (containing the stomach). If the diaphragm is not intact, it can compromise the ability of the lower oesophageal sphincter (LES) to prevent acid reflux. A hiatal hernia may decrease the sphincter pressure necessary to prevent reflux.
Whether or not the hernia is an initiating factor in GORD, it plays a role in sustaining GORD, accounting for the chronicity of the disease.
-
Visceral hypersensitivity
A subset of subjects with GORD symptoms has been shown to experience hypersensitivity to pain in the absence of excessive oesophagal acid exposure.
Some patients with normal oesophagal acid exposure might experience symptoms of GORD as a result of visceral hypersensitivity. The mechanisms underlying this impaired visceral perception are still unclear.
-
Impaired mucosal resistance
The ability of the oesophagal mucosa to withstand injury is a determining factor in the development of GORD.
The oesophagal mucosa contains several structural and functional components that serve as a protective defence against noxious luminal substances. 2 notable ones are the weak pre-epithelial defence and the epithelial defence.
Symptoms of Gastro Oesophageal Reflux Disease
The typical clinical presentation of GORD is :
- Heartburn
Heartburn is defined as a retrosternal burning sensation or discomfort that may radiate into the neck and typically occurs after the ingestion of meals or when in a reclined position
- Regurgitation
Regurgitation is a retrograde migration of acidic gastric contents into the mouth. However, GORD can also present with various other symptoms that include:
- Difficulty swallowing (Dysphagia)
- Pain when swallowing (odynophagia)
- Belching
- Epigastric pain
- Nausea
GORD presentation is considered to be atypical when patients present with extra-oesophagal symptoms such as chest pain, chronic cough, asthma, laryngitis, dental erosions, dysphonia, hoarseness, and globus sensation (persistent sensation of a lump in the throat).
Investigation for Gastro Oesophageal Reflux Disease
There is no gold standard test available.
-
Proton pump inhibitor (PPI) trial
GORD can be presumptively diagnosed in most patients presenting with typical symptoms of heartburn and regurgitation unless there are associated alarm symptoms that include dysphagia, odynophagia, anaemia, weight loss, and hematemesis.
Most patients can be initiated on empiric medical therapy with proton pump inhibitors (PPIs) without further investigations with a response to treatment confirming the diagnosis of GORD.

-
Esophagogastroduodenoscopy (EGD)
Patients presenting with typical symptoms associated with any one of the alarm symptoms should be evaluated with an EGD to rule out complications of GORD. These include erosive esophagitis(inflammation, irritation, or swelling of the lining of the oesophagus), Barrett’s oesophagus (when the healthy oesophagal epithelium is replaced with cancer-causing columnar cells), oesophagal stricture, and oesophagal adenocarcinoma or rule out peptic ulcer disease.
-
Ambulatory oesophageal reflux monitoring
This is used in assessing the correlation of symptoms with abnormal acid exposure. It is indicated in medically refractory GORD and patients with extra oesophagal symptoms suspicious for GORD.
A small tube with a pH sensor at the tip, worn for 24 hours, is sent through the nose into the oesophagus to measure how much acid is exposed to the oesophagus. Results are sent to a portable computer for analysis.
Complications of Gastro Oesophageal Reflux Disease
-
Erosive Esophagitis (EE)
This is characterized by erosions or ulcers of the oesophageal mucosa. Patients depending on the degree of esophagitis is endoscopically graded using the Los Angeles esophagitis classification system, which employs the A, B, C, and D grading system based on variables that include length, location, and circumferential severity of mucosal breaks in the oesophagus.
-
Oesophageal Strictures
Chronic acid irritation of the distal oesophagus can result in scarring of distal the oesophagus leading to the formation of a peptic stricture. Presenting symptom is usually oesophageal dysphagia or food impaction.
-
Barrett Oesophagus
This complication occurs as a result of chronic pathological acid exposure to the distal oesophagal mucosa leading to a histopathological change of the distal oesophagal mucosa from its normal stratified squamous epithelium to metaplastic columnar epithelium.
Barrett’s oesophagus is more commonly seen in Caucasian males. Age above 50 years, obesity, and a history of smoking are predisposing factors in the development of oesophageal adenocarcinoma.
Current guidelines recommend the performance of periodic surveillance endoscopy in patients with a diagnosis of Barrett’s oesophagus.
Diagnosing Gastro Oesophageal Reflux Disease
The diagnosis of GORD is made solely based on presenting symptoms or in combination with other factors such as responsiveness to antisecretory therapy, esophagogastroduodenoscopy, and ambulatory reflux monitoring.
Treatment for Gastro Oesophageal Reflux Disease
The goals of managing GORD are:
- To address the resolution of symptoms.
- Prevent complications such as esophagitis, Barrett’s oesophagus, and oesophagal adenocarcinoma.
Treatment options include
-
Lifestyle modifications
Healthy eating and maintenance of ideal weight cannot be over-emphasized, as it is the cornerstone in GORD management. Obesity has been implicated as a significant risk factor in the development of GORD.
-
Medical management with antacids and antisecretory agents
When lifestyle modifications fail, medical therapy is considered using:
-
- H2 receptor antagonist (H2RA) e.g. Cimetidine
- Proton pump inhibitor (PPI) e.g. Omeprazole, esomeprazole.
-
Surgical therapies
Laparoscopic Nissen fundoplication is the gold standard surgical treatment in the management of GORD patients. (In this procedure, the top of your stomach is sewn around your oesophagus).
However, given the rapid prevalence of obesity worldwide, gastric bypass surgery is becoming the most common surgical treatment for GORD.
Surgery is done for persons who are refractory, non-compliant or experience side effects with medical therapy
-
Endoluminal therapies
The current available endoluminal therapies include:
-
- Magnetic sphincter augmentation (MSA)
Here through laparoscopic surgery, a flexible band of magnetic titanium beads are placed around the oesophagus. This creates pressure on the oesophagus, helping hold it closed and preventing food and stomach acid from refluxing.
-
- Transoral incisionless fundoplication
This is a minimally invasive procedure done through the mouth without an external incision. Here, folding the fundus around the opening between the stomach and the oesophagus is done to reinforce the area thus preventing the stomach acid from coming up into the oesophagus. Fundoplication helps create a new barrier to reflux from the stomach.
Conclusion
It’s important to note that there’s a very real distinction between occasional heartburn (which may not need medical intervention) and GORD. Most people experience heartburn from time to time, and in general, occasional heartburn isn’t a cause for concern.
But if you’ve been experiencing heartburn more than twice a week, and especially if you’ve also been experiencing a chronic cough and chest pain, you might be dealing with GORD.it is important to consult your Gp for a proper assessment.

