Gastric sleeve or sleeve gastrectomy surgical intervention in obesity is today the most effective treatment method in high-level obesity management.
Obesity leads to serious health consequences such as cardiovascular disease (mainly heart disease and stroke), type 2 diabetes, musculoskeletal disorders like osteoarthritis, and some cancers (endometrial, breast and colon). These conditions cause premature death and substantial disability.
Gastric sleeve interventions not only ensure body weight reduction, but effective and sustained weight loss also may influence dietary habits and thus improves metabolic syndrome and obesity-related diseases. And it is the 1st step of duodenal switch.
To understand gastric sleeve surgery, a little knowledge of the anatomy and functions of the stomach will help make things clearer.
The stomach is a muscular, saclike, distensible expansion of the digestive system, between the oesophagus and the small intestine. It is located in the anterior part of the abdominal cavity and may take varying shapes, depending on the build, posture of the person and the state of fullness of the organ.
In adults, the stomach has a capacity of about 2.5 ounces (0.07L) when empty and relaxed but can expand to hold about 1 quart of food (about 1.8L) and the functions include viz:
- The temporary storage of food
The upper portions of the stomach (cardia, body, and fundus) relax as food enters to allow for the stomach to hold increasing quantities of food.
- Partial chemical and mechanical digestion of food
The lower portion of the stomach contracts in a rhythmic fashion (mechanical digestion) to aid with the breaking down of food and mixes it with stomach juices, hydrochloric acid (HCl) and the enzyme pepsin (chemical digestion) which also serve to break food down and prepare the mixture, called chyme for further digestion. Mixing waves are produced and this increases in intensity as the chyme reaches the lower portion of the stomach. With each wave, the pyloric sphincter allows small quantities of sufficiently liquefied/ broken down chyme into the small intestine (gastric emptying) where the main digestion takes place.
- Production of hormones and enzymes that help digest food
Stomach juices are liquids naturally secreted by the fundal portion of the stomach for the chemical purposes of digestion and include hydrochloric acid (HCl) and the enzyme pepsin. In addition to these, the stomach also produces an intrinsic factor that allows for the absorption of vitamin B12 (cobalamin) which plays an important role in the production of red blood cells and neurological functions.
The stomach also produces the hormone, ghrelin(also called the hunger hormone) more at the fundal part. Its levels typically rise before a meal, when the stomach is empty, and then decrease shortly after, when your stomach is full. It also controls gastric motility and the release of stomach acid.
The chyme produced in the stomach is then emptied into the small gut(Gastric emptying) for further digestion, however, the rate is heavily dependent on the type of food being consumed as carbohydrates are broken down in the stomach relatively fast, as are proteins, as opposed to fats such as triglycerides which take longer to be processed by the stomach.
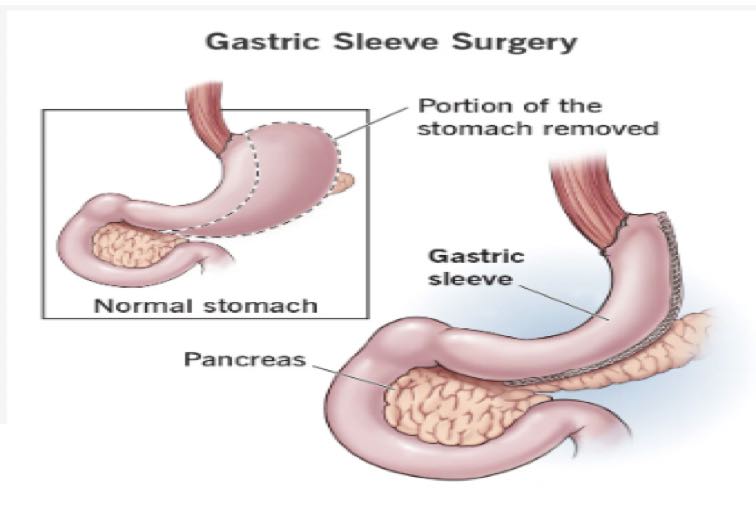
What is a gastric sleeve or sleeve gastrectomy?
Gastric Sleeve is the most performed bariatric surgery in the past 15 years and has become the most popular bariatric procedure worldwide. It involves the removal of about 80% of some portions of the stomach (from the fundus to the body of the stomach thus transiting the stomach from a long stretchable organ to a narrow sleeve or tubular shape that resembles a banana.
This leaves one with less space for food and more importantly, it affects the gut hormone that affects hunger, ghrelin (also called the hunger hormone), the sensation of fullness, and blood sugar control and also helps to reduce your set point.
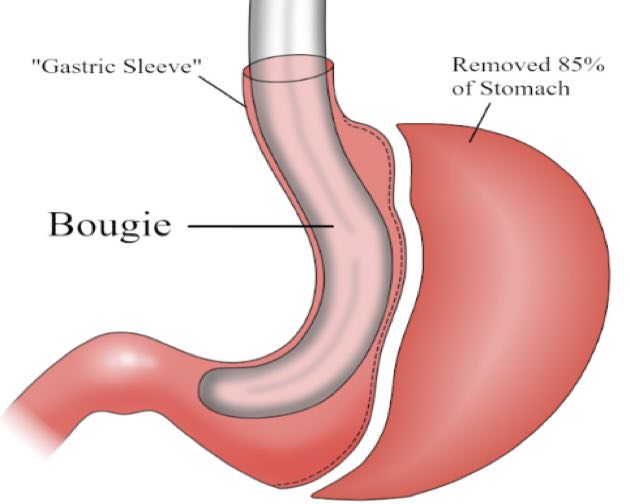
In the gastric sleeve, a soft plastic tube (called the Bougie) is inserted through the mouth to the oesophagus under endoscopy guidance to outline and form the new stomach. The bougie comes in different sizes measured in the unit called ‘French ‘ e.g. 50F, 40F, 36F etc. This helps the surgeon guide the cutter and place the stapler that holds the new stomach.
Please, note that gastric sleeve is not the same procedure as endoscopic sleeve gastroplasty.
In gastric sleeve(sleeve gastrectomy), 80-85% of the stomach is cut along the great curvature and completely removed from the body, whereas in the endoscopic sleeve gastrectomy 70-80% of the stomach is isolated from the rest of the stomach by sewing it along the great curvature.
Facts about gastric sleeve
- Effective and sustained weight loss.
- Essentially still the normal anatomy.
- There is improvement in metabolic syndrome and obesity-related diseases.
- The procedure is irreversible and no adjustment after the surgery.
- No Malabsorption.
- No foreign objects are put inside the body.
- There is a loss of about 60% of excess body weight (EBW).
- Increased risk of reflux and oesophagal cancers if untreated reflux continues.
- There is a need to undergo long-term endoscopic surveillance to monitor silent refluxes.
- A lower rate of diabetic remission is noted.
- The tendency for re-sleeving or revision surgery.
- Less than 2% of major complication rate.
- Ist step to duodenal switch.
- Can still take Non-steroidal anti-inflammatory drugs(NSAID)
Who is qualified for gastric sleeve surgery?
The surgery is recommended for people who are obese and suffering from medical conditions caused by their weight. A general guideline to whether a patient can undergo weight loss surgery is based on their body mass index (BMI).
Adults who have a BMI of 40 or more are usually considered, and adolescents who have a BMI of 35 and obesity-related illness. Adults may be eligible for the gastric sleeve procedure if they meet the following conditions:
- That you have sever obesity (Class 111) This is determined by the body mass index (BMI) which is calculated by weight and height and related health conditions. Class III obesity means a BMI of more than 40.
- BMI of between 35- 39(with a least one illness)
- Suffer from obesity-related illnesses such as diabetes, back pain, sleep apnoea, joint problems or another issue
- Adolescents may be eligible for the gastric sleeve procedure with a lower BMI, and in addition, suffer from a severe obesity-related illness
- Healthy enough to undergo the operation.
- Had other failed attempts at medical weight loss for at least 6 months. (You may be required to spend three to six months on a medically supervised weight loss plan before your insurance company will approve and cover your surgery.
- Physically and mentally prepared for the surgery and recovery process.
- No uncontrolled psychiatric condition.
Before qualifying for weight loss surgery, you’ll meet with a team of dietitians, psychologists and other medical specialists for counselling and screening.
Preparing for gastric sleeve
After passing the health screening and qualifying for bariatric sleeve surgery, the next step will be a two-week liquid diet (low carbohydrate, low fat and high protein low calorie diet). The surgeon gives specific guidelines to follow. The purpose is to viz.
- Lose some of the fat in your abdomen and your liver to make the surgery safer.
- Helps clean the stomach. (Having food or liquid left in your stomach during the surgery could cause unpleasant or even dangerous side effects).
- Decrease the size of the liver (Large livers obstruct access to the surgery site).
- Mindset and mental awareness are created thus helping in the mental shift.
- Changes the current habit /cravings.
- Helps patient’s to adapt post-surgery.
You’ll be asked not to eat or drink anything for 12 hours before your operation. That’s to make sure your stomach is empty during the procedure. Having food or liquid left in your stomach during the surgery could cause unpleasant or even dangerous side effects.
Complications
- Early complications
-
- Leakage from new connection.
- Nausea and vomiting.
- Blood clotting.
- Late complications
-
- Gallstone formation.
- Gout flare.
- Vitamin and mineral deficiencies.
- Hair shedding.
- Heartburn or acid reflux.
Why does gastric sleeve surgery fail?
The gastric sleeve fails when:
- There is a failure to achieve the expected weight.
- Weight regain post-surgery
Weight is controlled by the brain called the hypothalamus via several robust and intricate mechanisms.It senses our peak fat mass through a chemical called leptin and always tries to go back to that level. Weight gain post surgery depends on viz:
-
- The right surgery
-
-
- The bougie size used can go a long way in determining the success of the surgery. From Swedish obesity studies, a drop in bougie size from 50 French to 36 French resulted in 10% better excess weight loss.
-
Bougie is a soft plastic tube inserted through the mouth into the oesophagus to outline and form the new stomach. The surgeon uses the bougie to guide the cutter and stapler.
-
-
- Converting Lap band to sleeve.
-
The oesophagus may expand in response to the band thus creating an extra stomach making the sleeve not to be effective.
-
- Right patient behaviours
-
-
- Snaking and grazing on high-calorie carbohydrates.
- Wrong food choice.
- Excessive alcohol intake.
- Use of energy drinks.
- Right caloric intake (less than 1000) – more calories in carbohydrates, 90% of the energy is absorbed or retained, while fat food (80%) and Proteins-70%. Also proteins cannot be converted to Fat.
- Not exercising.
- Mistaking reflux for Hunger.
-
-
- The right follow up
Typically, one attends four to six follow-up meetings during the first post-surgery year. Then visits are scheduled at six to twelve-month intervals for an indefinite period. First visit: Scheduled 2-3 weeks after bariatric surgery. Second visit: Scheduled 4-5 weeks after bariatric surgery.
-
- The use of an antidepressant called mirtazapine (Avanza)-This drug has a bad reputation for increased acid reflux and sugar craving and should not be used post-op. Patients on this put on up to 15 kg weight.
- Steroid prednisolone.
- Should not get pregnant 1-year post-op.
- There are intolerable side effects (reflux and vomiting).
Management of weight regain post-gastric sleeve
- Diet review
Dietician will work with the patient to rejig the diet.
- Rice cream assessment
In this test, patients are asked to eat as much of a can of rice pudding at a consistent pace until they recognize:
-
- The point at which they are feeling satisfied (Satiety volume).
- The point at which they no longer eat more (Maximum tolerated volume).
In the majority of patients whose capacity approaches a whole can of rice cream, weight regain is common.
- Barium meal
-
- Helps see the shape of the stomach.
- Endoscopy
The sleeve is evaluated for hiatus hernia and reflux.
- Back on track course/counselling
- Sleeve revision
-
- When BMI is back in a dangerous range.
- When the trajectory of weight gain is continuing.
- Expected weight loss is below 40%.
- When new or old comorbidities are beginning to appear.
- When there is a logically correctable problem like a large pouch.
- When other measures fail.
- Alternative to re-sleeve
Omega loop- mini gastric bypass is an alternative to re-sleeving. Omega-Loop is sometimes referred to as mini gastric bypass as it involves only making one anastomosis (connection) instead of two like during Roux-en-Y. During Omega-Loop, the stomach pouch is reduced in size and interconnected to the small intestine.
-
- The stomach empties very rapidly which rapidly switches off hunger.
- Profound dumping syndrome if wrong choices of food are made.
- Profound effects on T2 DM
Conclusion
Considering gastric sleeves as surgical management of obesity? You have not made a wrong choice. The gastric sleeve is the most commonly performed weight loss surgery in the U.S. and worldwide. More than half of bariatric surgeries performed in the U.S. each year are sleeve gastrostomies
In the gastric sleeve, the stomach anatomy is essentially normal. Reducing the size of the stomach simply restricts the amount of food one eats at a sitting, making one fuller and also reducing the number of hunger hormones that the stomach can produce thus resetting the ‘appetite thermostat.’

