Gastric bypass, also known as a roux-en-y gastric bypass (RYGB), is the gold standard weight loss surgery. This is due to its lasting popularity and reducible results. Obesity is considered an epidemic all over the world and it is recognized as one of the major public health problems.
With morbid obesity, the body will always try to get back to its peak weight and this brings into play multiple powerful mechanisms. When other measures to control weight fail, Bariatric surgery becomes one of the most effective surgical management.
What is Roux-en-Y Gastric Bypass?
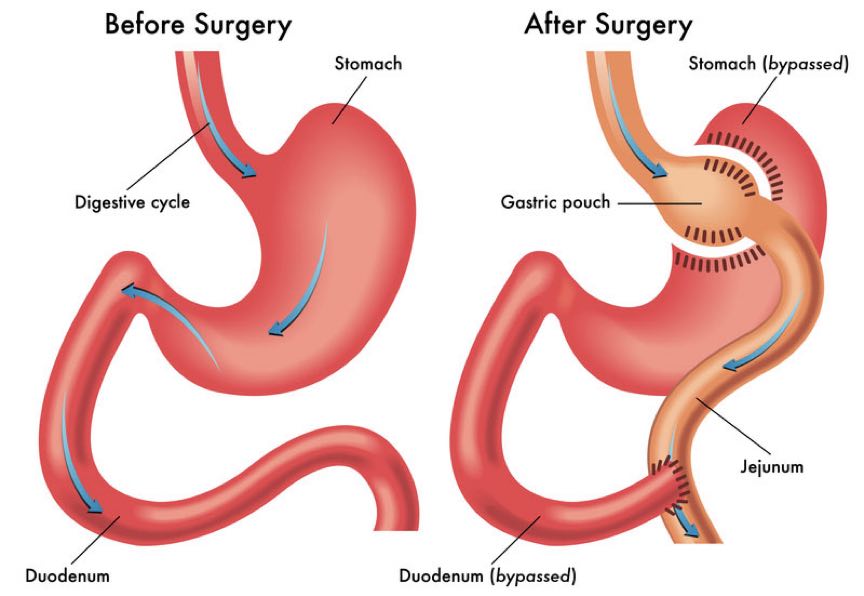
The Roux-en-Y gastric bypass (RYGB) is the most frequently performed weight loss procedure. During the first part of RYGB, a small pouch is created in the stomach with staples. This step restricts the amount of food the patient can consume to approximately one ounce. The remaining, larger part of the stomach is then separated from the pouch but is not removed. The second step of this procedure involves dividing the small intestine just below the duodenum. Next, the second section of the small intestine, the jejunum, is brought up and is connected to the newly created pouch. The duodenum is then reconnected to the new intestinal limb giving the intestine the Y shape for which the procedure is named. By bypassing the duodenum, the absorption of nutrients and calories are prevented, resulting in significant weight loss.
After RYGB, levels of gastrointestinal hormones, such as glucagon-like peptide-1 (GLP-1) and peptide YY (PYY), are increased, possibly contributing to satiety, weight loss, and remission of diabetes. Increased insulin sensitivity is evident immediately postoperatively, before significant weight loss occurs, suggesting that neurohormonal factors are prominent in the remission of diabetes. A change in the gut microbiome may also contribute to changes in weight after RYGB.
Types of Roux-en-Y (RYGB) Gastric Bypass
-
Gastric bypass, Roux-en-Y (RYGB, proximal)
This variant is the most commonly employed gastric bypass technique and is by far the most commonly performed bariatric procedure in the United States. The small intestine is divided approximately 45 cm (18 in) below the lower stomach outlet and is re-arranged into a Y-configuration.
In the proximal version, the Y-intersection is formed near the upper (proximal) end of the small intestine.
-
Gastric bypass, Roux-en-Y (RYGB, Distal)
The Y-connection is moved further down the gastrointestinal tract, and the amount available to fully absorb nutrients is progressively reduced, traded for greater effectiveness of the operation. The Y-connection is formed much closer to the lower (distal) end of the small intestine, usually 100–150 cm (39–59 in) from the lower end, causing reduced absorption (malabsorption) of food. Primarily of fats and starches, but also various minerals and fat-soluble vitamins. The unabsorbed fats and starches pass into the large intestine, where bacterial actions may act on them to produce irritants and malodorous gases. These larger effects on nutrition are traded for a relatively modest increase in total weight loss.
Facts About Gastric Bypass
- There is a benefit of long-term sustained weight loss.
- Surgery is done on both the stomach and the intestine.
- Intermediate and strong metabolic improvements in metabolic syndrome obesity-related diseases.
- It has long-term data. It’s been around since the 1950s
- It is potentially reversible.
- The estimated body weight loss is 70-80% In 1 -2 yrs.
- High risk of Vitamin deficiencies and anaemia
- High risk of dumping syndrome.
Normally, the pyloric valve at the lower end of the stomach regulates the release of food into the bowel. When a gastric bypass is done, this function is lost and when the patient eats sugary food, the sugar passes rapidly into the intestine, where it gives rise to a physiological reaction called dumping syndrome. The reacts to the sugar by flooding the intestines with gastric content in an attempt to dilute the sugars. An affected person may feel the following viz:
-
- Nausea and vomiting.
- Flushing.
- Sweating.
- Light headaches.
- Watery diarrhoea.
- The patient may never take Non- Steroidal Anti-Inflammatory Drugs(NSAIDs) like Aspirin, Ibuprofen etc or use tobacco products due to risks of marginal ulcers (marginal ulcers form at the point where the new stomach is attached to the intestine) the intestine here does not have protective mechanism as the proximal intestines next to the stomach.
Who is Suitable for the Surgery?
- Have a body mass index (BMI) of more than 40 kg/m2 or a BMI of more than 35 kg/m2 plus a serious complication (e.g., Diabetes, Hypertension, Obstructive sleep apnea, high-risk lipid profile).
- Have acceptable operative risk.
- Be well-informed and motivated.
- Have unsuccessfully tried all reasonable nonsurgical methods to lose weight and manage obesity-associated complications.
Effects of Gastric Bypass
A normal stomach can stretch, sometimes to over 1000 mls, while the pouch of the gastric bypass may be 15 mls in size. When the patient ingests just a small amount of food, the first response is a stretching of the wall of the stomach pouch, stimulating nerves that tell the brain that the stomach is full.
The patient feels a sensation of fullness as if they had just eaten a large meal. Food is first churned in the stomach before passing into the small intestine. When the lumen of the small intestine comes into contact with nutrients, several hormones are released viz:
- Cholecystokinin from the duodenum.
- PYY/GLP-1 from the ileum.
These hormones inhibit further food intake. Also Ghrelin, a hormone, that is released in the stomach stimulates hunger and food intake. Changes in circulating hormone levels after gastric bypass have been thought to produce reductions in food intake and body weight in obese patients.
Contraindications
Contraindications include:
- An uncontrolled psychiatric disorder such as major depression.
- Current drug or alcohol abuse.
- Cancer that is not in remission.
- Another life-threatening disorder.
- Inability to comply with nutritional requirements, including life-long vitamin replacement (when indicated).
Complication / Risks
As with any major surgery, gastric bypass and other weight-loss surgeries pose potential health risks, both in the short term and long term.
-
Short Term Risks
Risks associated with the surgical procedure are similar to any abdominal surgery and can include:
-
- Excessive bleeding.
- Infection
- Adverse reactions to anaesthesia.
- Blood clots.
- Lung or breathing problems.
- Leaks in your gastrointestinal system.
-
Longer Term Risks
-
- Bowel obstruction.
- Dumping syndrome causes diarrhoea, nausea or vomiting.
- Gallstones.
- Hernias.
- Low blood sugar (hypoglycemia).
- Malnutrition.
- Stomach perforation.
- Ulcers.
- Vomiting.
- Candy cane syndrome is a rare complication reported in bariatric patients following Roux-en-Y gastric bypass. It occurs when there an excessive length of the small intestine is left before the point of attachment of the intestine with the new stomach pouch, creating the possibility for food particles to lodge and remain in the blind redundant limb. This has been implicated as a cause of abdominal pain, nausea, and emesis after Roux-n-Y gastric bypass (RYGB) but remains poorly described.
4 Reasons Gastric Bypass Fails
- Big Stroma
The stoma is the opening from the pouch to the intestines. This opening is what permits food to pass through. If it is too large there will be no restriction to food passage no matter how small the pouch is. The food eaten travels freely into the small intestines.
The bypass works by offering both restriction and malabsorption, so a large stoma will jeopardize the weight loss because it will not give you any restriction. The ideal stoma opening is less than 18 mm.
- Sabotaging Feeding Behaviors
Gastric bypass has the advantage of allowing patients to lose weight in two ways. The restrictive component plus the malabsorptive component. Losing weight in the first few years is easy even if you are not very careful in choosing what you eat given the nature of the bypass.

But over time if habits aren’t changed weight can creep back up. Eating right after surgery maximizes the weight loss results from the beginning and also creates good habits that will last a lifetime.
Protein is key with all weight loss surgeries so be sure you have protein in every meal and snack you eat. Continue to keep meals separate from drinks as well, this is a rule that many patients forget over time and avoid high-calorie liquids.
Visit a bariatric nutritionist if possible, certain food combinations work best for weight loss and keeping you satiated throughout the day to better help you change your habits.
- Malabsorption
The malabsorptive component of the bypass is just as important as the restriction. The length of the limbs your surgeon leaves during surgery determines how much malabsorption you will have after surgery.
There is no one size fits all solution, the surgeon will determine the lengths once he is inside and measures the total length of your intestines and takes into consideration other factors like your BMI, co-morbidities you may have, the size of your pouch, etc.
For some patients, the malabsorption they have is not enough to help them keep the weight off long-term. As time goes by the body becomes more efficient and learns to absorb more so patients lose more of the malabsorptive component and are solely relying on the restriction the bypass offers and this may not be enough to maintain weight loss. Some patients may need more malabsorption added in the long run.
- Big Pouch
There is not one single technique for performing a gastric bypass. Surgeons use their criteria, experience, etc. to determine how the bypass will be done. This means that some surgeons give patients different size pouches. Having a pouch that is too large for you means you can eat too much food in one meal.
The restriction is one of the 2 components of a bypass and a very large pouch eliminates this important aspect. Initially, you may lose weight fine but over time if the pouch is too big you will most likely regain the weight.
Nutritional Deficiencies in Gastric Bypass
These are relatively common but often missed or not recognized.
- Secondary hyperparathyroidism
Following gastric bypass, absorption of calcium (which is primarily absorbed in the duodenum) is affected. Remember that the surgery bypasses the duodenum, although most patients can still achieve adequate calcium absorption by supplementation with vitamin D and calcium citrate.
Please note that calcium carbonate may not be absorbed if taken as a supplement because it requires an acidic stomach, which is bypassed to be absorbed.
- Iron Deficiency
Iron is absorbed from the duodenum, which is bypassed. The deficiency is worse during menstrual losses. Signs of deficiency include:
-
- Brittle nails.
- Inflamed tongue.
- Constipation.
- Depression.
- Headaches.
- Fatigue.
- Mouth lesions.
This is usually treated with iron supplements, especially with the fumarate form of iron (Iron fumarate) or the chelated forms. Note iron Sulphate can cause considerable gastric upset. And in severe forms of iron deficiency, parenteral iron administration is advised.
- Zinc deficiency
Signs and symptoms of Zinc deficiency are viz:
-
- Acne.
- White spots on the nails.
- Eczema.
- Hair loss.
- Depression.
- Amnesia.
- Lethargy.
- Vitamin B1 deficiency (Thiamine)
Signs and symptoms of vitamin B1 deficiency include viz:
-
- Heart failure.
- Memory loss.
- Numbness of the hands.
- Constipation.
- Loss of appetite.
This brings the risk of permanent neurological damage (i.e. Wernicke’s encephalopathy) to light if supplementation is not given.
- Vitamin B12 deficiency (Cobalamin)
Vitamin B12 deficiency is quite common after gastric bypass. Vitamin B12 requires intrinsic factors from the stomach mucosa to be absorbed. This becomes a big problem in gastric bypass with a small pouch. Vitamin B12 oral supplements may still not be absorbed thus leading to pernicious anaemia. Sublingual B12 (appears to be adequately absorbed. In cases where sublingual B12 does not provide sufficient amounts, injections may be needed.
- Deficiency of vitamin A
Deficiencies occur after bypass procedures or as a result of weight loss medications
- Protein Malnutrition
Many patients require protein supplementation during the early phases of rapid weight loss to prevent excessive loss of muscle mass. Hair loss is also a risk of protein malnutrition.
- Folate deficiency
Deficiency is also a common occurrence in gastric bypass surgery patients.
Conclusion
Gastric bypass is a life-changing surgery-not just the kilos are affected, but the health improves. For potentially life-threatening morbidly obese patients with type 2 Diabetes, a successful gastric bypass surgery means better-managed diabetes, improved chances of remission, reduced need for diabetic medication and a dramatically enhanced quality of life.
Patients need to be properly counselled and prepared for changes (complete life overhaul) and unexpected transformations after a gastric bypass, including changes in their relationship. A 2018 study found that of nearly 1,000 obese patients in relationships who had had bariatric surgery, 9% had divorced or separated within four years of their surgery –‘the bariatric divorce’.
More research is therefore needed to better understand the factors contributing to an observed increase in relationship breakdowns following bypass surgeries. Now the question is, “is bariatric surgery compromising healthy marriages or helping people get out of unhealthy relationships?

