Duodenal switch is a weight-loss surgery designed to treat people who have severe obesity. It combines a gastric sleeve (sleeve gastrectomy) with an intestinal bypass.
In the normal digestive system, food moves from the mouth through the oesophagus to the stomach where it is stored temporarily and broken down into smaller particles. These are moved into the pylorus (the muscular valve) that opens and closes during digestion.
Thus allowing partially digested food and other stomach contents to empty into the first part of the small intestine, called the Duodenum.
Here, the enzymes from the pancreas, and bile from the liver are secreted into the gut to aid in the digestion of food as it journeys the small intestine and later to the colon where fluid is absorbed and faeces is formed.
The goal of a duodenal switch operation is to modify the stomach and intestines to treat obesity and related diseases. The operations may make the stomach smaller and also bypass a portion of the intestine.
This results in less food intake and changes in how the body absorbs food for energy resulting in decreased hunger and increased fullness. These procedures improve the body’s ability to achieve a healthy weight.
What is Duodenal Switch (DS)?
This is the most successful operation for the treatment of obesity. Duodenal switch is a combination of 2 surgeries viz: gastric sleeve and Roux-en-Y surgery (RYGB).
Types of Duodenal Switch
- Biliopancreatic Diversion with Duodenal Switch (BPD-DS)
The stomach is first reduced in size by performing a gastric sleeve. In the gastric sleeve, a soft plastic tube (called the bougie) is inserted through the mouth to the oesophagus under endoscopy guidance to outline and form the new stomach.
The bougie comes in different sizes measured in the unit called ‘French ‘e.g. 50F, 40F, 36F etc. This helps the surgeon guide the cutter and place the stapler that holds the new stomach.
About 80-85% of the stomach is cut along the great curvature and completely removed. This limits the volume of food that can be taken.
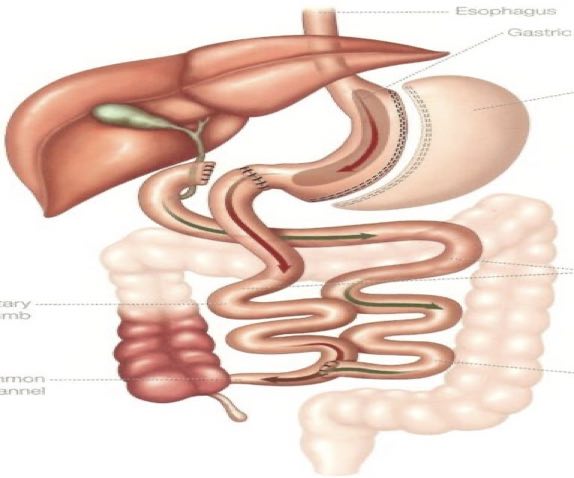
In the 2nd part of the surgery, the duodenum is divided about 3cm after the pylorus, thus preserving the pylorus, next, the small bowel is divided 10 feet from the last part of the small intestine and then attached to the new stomach thus allowing food to bypass a large part of the small intestine where calories and nutrients are normally absorbed.
The anastomosis can be tested by insufflating air through the nasogastric tube and repair sutures applied if there is a leak. The remaining intestine is reconnected back to itself approximately 5 feet from the entrance into the large intestine (ileo-caecal junction).
This reconnection allows the enzymes from the pancreas and the bile from the liver to mix with food to aid digestion before entering into the large intestine.
Following the completion of the anastomosis, the mesenteric window (Petersen window) is closed to prevent an internal hernia. After this has been completed, a routine cholecystectomy (gallbladder removal surgery) and liver biopsy may be performed if warranted.
- Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
This is a modification duodenal switch surgery (also called the modified duodenal switch or one anastomosis duodenal switch (OADS).
The modified duodenal switch is the newest option in bariatric surgery. It is based on the traditional duodenal switch but is modified to significantly decrease the side effects and the risks of complications that are associated with the traditional operation.
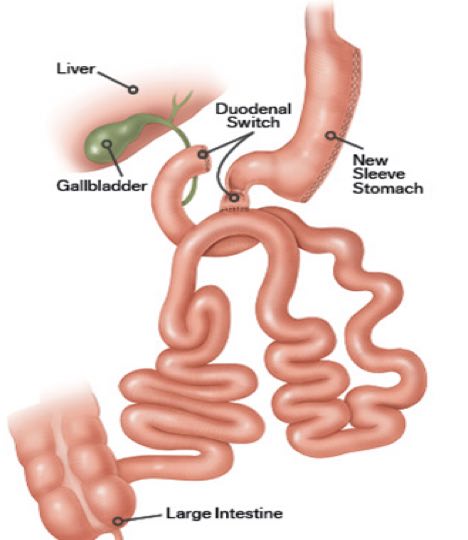
The operation starts the same way as the sleeve gastrectomy, making a smaller tube-shaped stomach. The first part of the small intestine is divided just after the stomach then a loop of the intestine is measured several feet from its end and is then connected to the stomach.
This is the only intestinal connection performed in this procedure.
Effects of Duodenal Switch
- Restrictions
A much less stomach sleeve means much less volume capacity. For the first few months after surgery, the stomach may be only about a quarter of a cup. As time goes on, most people can usually eat about a cup of food.
- Decreases hunger
There is usually no hunger at all for the first few weeks to months after surgery. Hunger does come back eventually for most people. When it does, it is usually less than before surgery and can be satisfied with much less food. As with gastric sleeve (sleeve gastrectomy) and Gastric bypass, switch operations reduce the “hunger hormone”, ghrelin.
- Causes dumping /rapid sensation of fullness
The intestines are much more sensitive than the stomach and this can cause unpleasant reactions to certain types of food. Usually, high-calorie foods, such as concentrated sugars and fats, are the type that causes problems. Dumping can include nausea, diarrhoea, cramping and low blood sugar. These unpleasant side effects help you stay away from junk food.
- Decreased ability to absorb calories if much food is consumed
After a switch operation, not all the calories in the food eaten are digested. This is a significant part of Switch operations, both the classic and the modified. This is why switch operations have a higher average weight loss than any of the operations, but it is also why the chance of malnutrition is higher.
Facts about Duodenal Switch Operation
- Higher average weight loss than gastric sleeve (Sleeve gastrectomy), Gastric bypass or Lap-Band.
- Better chance of controlling diabetes than a gastric sleeve (Sleeve gastrectomy), Gastric Bypass or Lap-Band.
- Does not have the ulcer risk of a gastric bypass.
- More complex surgery than sleeve gastrectomy, gastric bypass or lap-Band.
- The risk of intestinal obstruction, while rare, is higher than in Sleeve Gastrectomy or Lap-Band and similar to gastric bypass.
- Involves malabsorption which means a higher risk of metabolic disorders, diarrhoea, vitamin or mineral deficiencies and protein deficiency.
- It dramatically improves metabolic syndromes such as type 2 DM.
- It also has a higher rate of complications, but for people with more severe conditions, the benefits outweigh the risks.
Who is Qualified to Get a Duodenal Switch (DS)?
- BMI more or = 40 and BMI more or = 35 with at least one obesity-related comorbidity (such as diabetes mellitus, obstructive sleep apnea, hypertension, and severely limiting musculoskeletal issues).
- Unsuccessful non-operative weight loss treatments.
- Mental health clearance.
- No medical contraindications to surgery.
- Super obese patients with a BMI of more than 50 should be considered for DS.
- For patients who fail operative treatment with Roux en-Y bypass and gastric sleeve, biliopancreatic diversion with a duodenal switch should be considered.
Contraindications
Absolute contraindications to duodenal switch are viz:
- Pregnancy.
- Severe psychiatric illness.
- Eating disorders.
- Patient-related contraindications to undergo surgery (cardiovascular risk, anaesthetic risk).
- Substance misuse (alcoholism).
- Severe coagulopathies.
Complications of Duodenal Switch
-
Anastomotic leak
This is the most dreaded complication of any bariatric procedure because it increases overall morbidity to 61% and mortality to 15%. These patients may be asymptomatic, but they frequently present with.
-
- Tachycardia (abnormally rapid heart rate), is usually the first sign.
- Tachypnea (abnormally rapid breathing).
- Fever.
The diagnostic test of choice for an anastomotic leak should be a CT scan with oral and intravenous contrast. If the leak is acute (less than 5 days), they should return to the operating room for exploration with repair and placement of a distal feeding tube.
-
Bleeding
This can present as intraluminal (within the lumen) and extraluminal (outside the lumen). The incidence of bleeding has improved due to improved staple technology. Bleeding is more commonly seen with laparoscopic gastric bypass than in open procedures. Bleeding following surgery is treated at the surgeon’s discretion, depending on the patient’s clinical picture.
For intraluminal bleeding, endoscopic treatment may be necessary but is not very common. Patients who have extraluminal bleeding and are hemodynamically unstable (occurs when there’s abnormal or unstable blood pressure), and unresponsive to resuscitation will need to return to the operating room for exploration and repair.
-
Nutritional Deficiencies
Duodenal switch is the one bariatric procedure associated with the greatest perioperative malnutrition and metabolic-related complications. All patients must be on supplementation postoperatively. Common nutritional deficiencies that can be seen are:
-
- Iron deficiency anaemia.
- Protein-calorie malnutrition.
- Hypocalcaemia.
- Deficiency of fat-soluble vitamins.
- Vitamin B1, vitamin B12.
- Folate.
Close follow-up and laboratory studies are essential for these patients. If a nutritional deficiency is detected, dietary supplementation is extremely important.
Conclusion
With rising cases of obesity and their comorbidities, today’s management has also become complex. The duodenal switch is the most complicated but also the most effective bariatric surgery.
In addition to their ability to treat obesity, duodenal switch operations are very effective in treating diabetes, high blood pressure, sleep apnea and high cholesterol, among many other diseases.
These operations also can prevent future health problems. The benefits allow patients with obesity that choose to undergo treatment to enjoy a better quality of life and a longer lifespan.

