Coronary Artery disease (CAD) is a heart disease so it is important to understand how the heart works. The heart is a pump that pumps blood around the body, but it also has its supply called the coronary arteries (these are the first branches of the aorta-the main artery of the body).
They supply the heart muscles with oxygen-rich blood and they are 2 main branches that form a complex network of arteries that supply all areas of the heart viz:
- The left coronary Artery (LCA) – Has two branches:
-
- Left anterior descending (LAD)
- Left Circumflex (LCX) coronary arteries
- The Right Coronary Artery (RCA)
What Then is Coronary Artery Disease (CAD)?
Coronary artery disease (CAD) therefore is a condition that involves the impairment of blood flow through the coronary arteries. This is usually caused by a build-up of materials that adhere to the blood vessels especially fat, cholesterol etc.
Clinically Coronary artery disease (CAD) presents as thus:
-
Silent Ischemia
Occurs when the heart temporarily doesn’t receive enough blood (and thus oxygen), and the patient is unaware and doesn’t have symptoms.
-
Angina Pectoris
A clinical syndrome presenting as left chest pain and pressure due to a transient reduction in oxygenated blood flow to the heart following a reduction in flow through the coronary artery, but without tissue death.
So there is an imbalance between oxygen demand and supply. Angina pectoris can be:
-
- Stable
This happens when the heart muscle needs more oxygen than it’s getting at that moment e.g. during eating, exercising, emotional stress and exposure to cold. These are things that can increase the workload of the heart. Thus, the relationship between workload or demand and loss of blood supply is usually relatively predictable.
-
- Unstable
When one gets angina symptoms while doing very little or resting.
-
Acute Coronary Syndrome (ACS)
-
- Unstable Angina
This is clinically worsening angina (e.g., angina at rest or with increasing frequency and/or intensity of episodes).
-
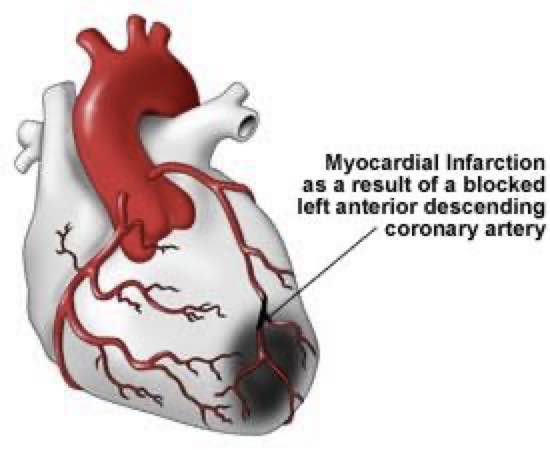
- Myocardial Infarction (Heart attack)
-
-
- Non-ST- elevation Myocardial infarction (NSTEMI)
- ST-elation Myocardial Infarction (STEMI)
-
-
Sudden Death
This is the sudden cessation of cardiac mechanical activity resulting in the stoppage of blood circulation to vital organs.
Causes of Coronary Artery Disease
Coronary artery disease is usually due to
-
Coronary Artery Atherosclerosis
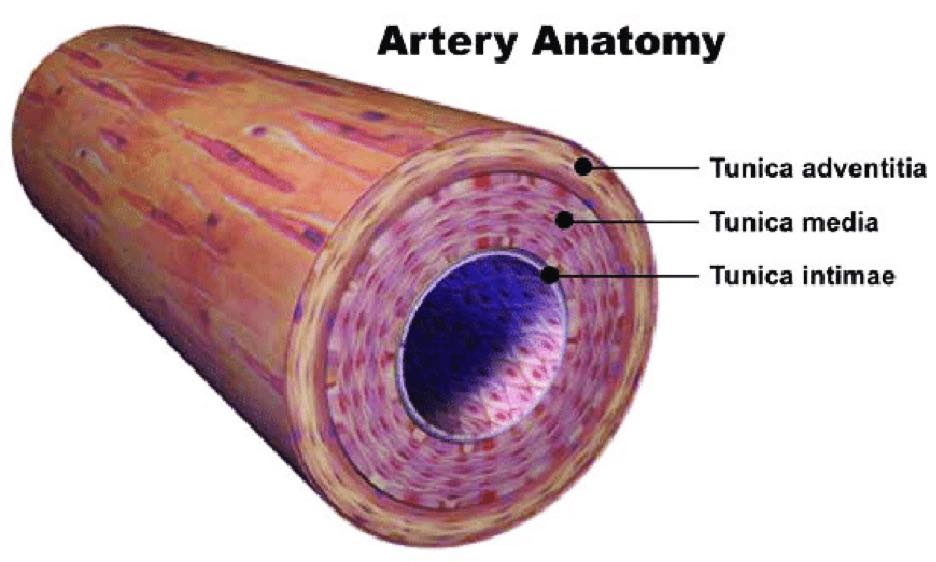
Here, plaques deposit in the intima layer of the coronary blood vessels (atherosclerosis) especially in the large and medium-sized coronary and then occlude the lumen. Atherosclerosis is often irregularly distributed in different vessels but typically occurs at points of turbulence (e.g. vessel bifurcations).
As the cholesterol plaque deposit in the intima layer of the coronary blood vessels grows, the arterial lumen progressively narrows, resulting in loss of blood supply thus causing chest pain. The degree of narrowing required to cause loss of blood supply varies with oxygen demand.
-
Coronary Artery Disease (also called variant, print metal or Vasospastic angina)
Here, the pain from variant angina is caused by a spasm in the coronary arteries (which supply blood to the heart muscle) which increases the vascular tone and a marked reduction in blood flow.
This marked narrowing can trigger blood clot formation, causing tissue death or life-threatening irregular heartbeats. Spasms can occur in arteries with or without fatty deposits in the blood vessel.
The use of vasoconstricting drugs (e.g., cocaine, nicotine) and emotional stress also can trigger a coronary spasm.
-
Vascular Endothelial Dysfunction
This can promote atherosclerosis and contribute to coronary artery spasms. Endothelial dysfunction is now also recognized as a cause of angina in the absence of epicardial coronary artery narrowing or spasm. (Arteries that run along the heart’s surface)
-
Coronary Artery Embolism, Dissection, Aneurysm
This is a non-traumatic tear in the coronary intima with the creation of a false lumen. Blood flowing through the false lumen expands it and restricts blood flow through the true lumen thus causing decreased blood flow to the heart and tissue death.
-
Vasculitis (e.g. in Systemic Lupus Erythromatosis (SLE) and Syphilis)
Vasculitis means inflammation of the blood vessels.
Risk Factors of Coronary Artery Disease
- Type 2 Diabetes
- Dyslipidemia (abnormal amounts of Lipids)
-
- High Total Cholesterol.
- High Triglycerides.
- Low High-Density Lipoproteins (HDL)
- High Low-Density Lipoproteins (LDL))/the variant Lipoprotein A.
- Smoking
Carbon monoxide, nicotine, and other substances in tobacco smoke can promote atherosclerosis and trigger symptoms of coronary artery disease.
- Obesity
Although obesity on its own is a risk factor for CAD and is linked to many other risk factors for CAD, such as diabetes, and high cholesterol.
- Physical Inactivity
The heart is a muscle and, like any other muscle, benefits from exercise. A strong heart can pump more blood around your body with less effort.
- High Level of Apo Protein B (Apo B)
These are proteins that help carry fat and cholesterol through the body. A high level of apo B may identify increased risk when total cholesterol or LDL level is normal.
- High Blood Levels of C-reactive Protein (CRP)
This is a substance produced in the liver that responds to inflammation. A high blood level of C-reactive protein indicates plaque instability/ inflammation and may be a stronger predictor of the risk of ischemic events than high levels of LDL.
Investigations for Coronary Artery Disease
Serial ECG or EKG
ECG is the most important test that should be done within 10 min of the presentation. It is the centre of the decision pathway because fibrinolytic (drugs that dissolve blood clots) and urgent cardiac catheterization are indicated for patients with acute STEMI but may increase the risk for those with NSTEMI.
For STEMI, initial ECG is usually diagnostic, showing ST-segment elevation ≥ 1 mm in 2 or more contiguous leads.
Serial Cardiac Markers
These are serum markers that indicate heart muscle cell injury. These markers are released into the bloodstream after the heart muscle is deprived of blood supply. The markers appear at different times after injury, and levels decrease at different rates. Sensitivity and specificity for myocardial cell injury vary significantly among these markers, but the troponins (cTn) are the most sensitive and specific and are now the markers of choice.
Recently, several new, highly sensitive assays of cardiac troponins (hs-cTn) that are also very precise have become available. These assays can reliably measure troponin levels (T or I) as low as 0.003 to 0.006 ng/mL (3 to 6 pg/mL); some research assays go as low as 0.001 ng/mL (1 pg/mL).
There are 2 classes:
-
- Cardiac enzymes (e.g., CK-MB [creatine kinase MB isoenzyme])
- Cell contents (e.g., Troponin I, Troponin T and Myoglobin)
-
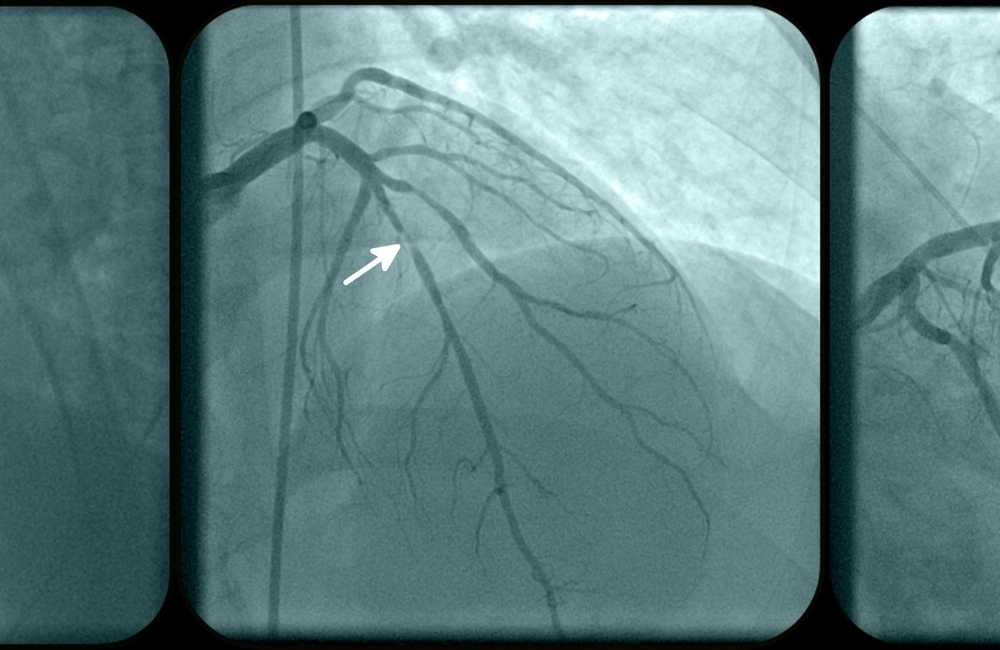
Immediate Coronary Angiography
This is especially for patients with STEMI or complications (e.g., persistent chest pain, hypotension, markedly elevated cardiac markers, unstable arrhythmias)
Most often combines diagnosis with percutaneous coronary intervention (PCI—i.e., angioplasty, stent placement). When possible, emergency coronary angiography and PCI are done as soon as possible after the onset of acute myocardial infarction (primary PCI).
-
Delayed Angiography
It is usually done within 24 to 48 hours for patients with NSTEMI or unstable angina without the complications noted above.
Treatment for Coronary Artery Disease
Treatment generally aims to reduce cardiac workload by decreasing oxygen demand and improving coronary artery blood flow and in long term – halt and reverse the atherosclerotic process.
Medical Treatment
Medical management of patients with CAD depends on symptoms, cardiac function, and the presence of other disorders.
-
- Antiplatelet drugs to prevent clot formation
- Statins to lower LDL cholesterol levels (improving short-term and long-term outcomes probably by improving athermanous plaque stability and endothelial function).
- Beta-blockers are effective in reducing symptoms of angina (by reducing heart rate and contractility, decreasing myocardial oxygen demand) and reducing mortality post-infarction, especially in the presence of post-myocardial infarction (MI) LV dysfunction.
- Calcium channel blockers are also helpful, often combined with beta-blockers in managing angina and hypertension but have not been proven to reduce mortality.
- Nitrates modestly dilate coronary arteries and decrease venous return, decreasing cardiac work and relieving angina quickly. Longer-acting nitrate formulations help decrease angina events but do not decrease mortality.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are most effective in CAD patients with left ventricular LV dysfunction.
-
Surgical Interventions
-
- Percutaneous coronary intervention (PCI)
PCI is indicated for certain patients with acute coronary syndrome (ACS) or with stable ischemic heart disease who have angina despite optimal medical therapy.
-
- Drug-eluting stents
Here the stent releases an antiproliferative drug (e.g., zotarolimus) over several weeks. Now, most PCI is done with stents, and about three-fourths of all stents used in the US are drug-eluting.
-
- Coronary artery bypass grafting (CABG)
CABG uses arteries (e.g., internal mammary, radial) whenever possible, and if necessary, sections of autologous veins (e.g., saphenous) to bypass diseased segments of the coronary arteries. At 1 year, about 85% of venous bypass grafts are patent, and after 5 years, one-third or more are completely blocked.
However, after 10 years, as many as 97% of internal mammary artery grafts are patent. Arteries also hypertrophy to accommodate increased flow. CABG is superior to PCI in patients with diabetes and patients with multivessel disease amenable to grafting.
Conclusion
Coronary artery disease (CAD is the leading cause of death in both sexes and prevention involves modifying atherosclerosis risk factors (see above) smoking cessation, weight reduction, a healthful diet, regular exercise, modification of serum lipid levels, and control of hypertension and diabetes.
Antihypertensive should be used to achieve the goal of blood pressure while modification of serum lipid levels (particularly with statins) may slow or even partially reverse the progression of CAD.