Congestive heart failure (CHF), also known as heart failure (HF), is a terrifying diagnosis for the patient! This doesn’t mean that the heart has failed or is about to stop working.
However, it is a serious condition in which the heart doesn’t pump blood as efficiently as it should and as a result, can’t keep up with the body’s demands. Also, blood returns to the heart faster than it is pumped out thus causing the heart to become congested.
Although about one-third of ambulatory patients with heart failure do not manifest pulmonary or systemic congestion, hence the preference of the term Heart failure over Congestive heart failure.
This pumping problem means that there is not enough oxygen-rich blood to support other organs of the body. Heart failure, therefore, results when the heart cannot keep up with its workload.
What is congestive heart failure (CHF)?
Congestive heart failure (CHF) develops when the heart fails to pump blood at a rate commensurate with the requirements of the metabolizing tissues. It is a syndrome of ventricular dysfunction that is chronic and progressive thus, resulting from:
- The ventricles are unable to pump blood hard enough during systole or cardiac contraction.
- Inability to fill up during diastole (when the heart rests).
- Or both.
At first, the heart tries to make up for this by:
- Enlarging
The heart stretches to contract more strongly and keep up with the demand to pump more blood. Over time this causes the heart to become enlarged.
- Developing more muscle mass
The increase in muscle mass occurs because the contracting cells of the heart get bigger. This lets the heart pump more strongly, at least initially.
- Pumping faster
This helps increase the heart’s output.
The body also tries to compensate in other ways viz:
- The blood vessels narrow to keep blood pressure up, trying to make up for the heart’s loss of power.
- The body diverts blood away from less important tissues and organs (like the kidneys), the heart and the brain.
These temporary measures mask the problem of heart failure, but they don’t solve it. Heart failure continues and worsens until these compensating processes no longer work.
Classification of congestive heart failure
Several classification systems are used to characterize heart failure according to the pathophysiology of heart failure viz:
-
Systolic versus diastolic heart failure
In Systolic dysfunction, the left ventricular ejection fraction (Ef) is reduced and there is also depressed contractility of the heart. Whereas in Diastolic dysfunction, the left ventricular ejection is preserved but there is an abnormality in myocardial relaxation or excessive myocardial stiffness.
The ejection fraction is the fraction of blood pumped out of a ventricle with each beat. The term ejection fraction applies to both the right and left ventricles; one can speak equally of the left ventricular ejection fraction (LVEF) and the right ventricular ejection fraction (RVEF). Without a qualifier, the term ejection fraction refers specifically to that of the left ventricle.
-
Left-sided, right-sided or both (biventricular heart failure)
In left-sided heart failure, there is impaired left ventricular function with reduced flow into the aorta. While in right-sided failure, there is impaired right ventricular function with reduced flow into the pulmonary artery and lungs.
The most common cause of right heart failure is left heart failure, and mixed presentations are common, especially when the cardiac septum is involved (Biventricular heart failure).
-
Low output versus high output heart failure
In low-output heart failure, the cardiac output is low and there is an inadequate supply of blood flow to meet normal metabolic demands. Whereas, in high-output heart failure, the cardiac output is high and there is an excess requirement for oxygen and nutrients .so, the demand outstrips what the heart can provide.
Causes of high-output heart failure include:
- Severe anaemia.
- Overwhelming Gram-negative infection.
- Vitamin B1/thiamine deficiency (also called Beriberi).
- Thyrotoxicosis.
- Paget’s diseases.
-
The underlying physiology
This is based on the left ventricular ejection fraction. (EF)
| S/N | Reduced EF | Slightly reduced EF | Preserved EF |
| 1 | < 40 % | 41 -59% | > 50% |
-
- Heart failure with reduced ejection fraction (HFrEF).
- Heart failure with mid-range ejection fraction (HFmrEF).
- Heart failure with preserved ejection fraction (HFpEF).
-
The chronicity of heart failure
-
- Acute or chronic
Acute or decompensated heart failure is a term used to describe exacerbated or decompensated heart failure and refers to an episode in which a patient sustains a change in heart failure signs and symptoms that necessitates urgent therapy or hospitalization while Chronic refers to stable symptomatology in chronic heart failure.
-
The severity of symptoms of heart failure
-
- New York Heart Association Class (NYHA class)
- No Limitations to physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath).
- Slight limitations to physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, and dyspnea (shortness of breath).
- Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes fatigue, palpitation, or dyspnea.
- Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases.
- Killip class (severity of the symptoms in the acute setting after myocardial infarction).
- New York Heart Association Class (NYHA class)
-
The stage (progression of the disease) of congestive heart failure
The American College of Cardiology Foundation/American Heart Association (ACCF/AHA) classification: A, B, C, and D.
Here, the classification system was introduced to emphasize the natural history of heart failure syndrome and to identify opportunities to intervene earlier and prevent disease progression.
-
- Patient at high risk of developing HF but without structural heart disease or symptoms of heart failure (Hypertensive, Diabetes, Family history of cardiomyopathy).
- Patient with structural heart disease who has never developed signs/symptoms of HF (left ventricular hypertrophy, previous heart attacks).
- Patients with past or current symptoms of HF associated with structural heart disease (Patients with known structural heart disease and symptoms of breathlessness, fatigue, and reduced exercise tolerance).
- Patients with refractory (end-stage) diseases who require specialized treatment strategies such as mechanical circulatory support, continuous inotropic infusions, cardiac transplantation or hospice care (patients who have marked symptoms at rest despite maximal medical therapy
Causes of congestive heart failure
-
Cardiovascular changes that occur with normal ageing
Cardiovascular changes that occur with normal ageing help explain why HF incidence and prevalence increase with age. Arterial stiffening with increased afterload and peripheral resistance occurs with advancing age even in normotensive individuals. An increase in left ventricular mass that often occurs with ageing may lead to impaired ventricular diastolic filling.
-
Hypertension
Hypertension accounts for 39% of new HF cases in men and 59% of new cases in women. Chronic hypertension leads to left ventricular hypertrophy (LVH) which is a common pathway in the development of HF.
-
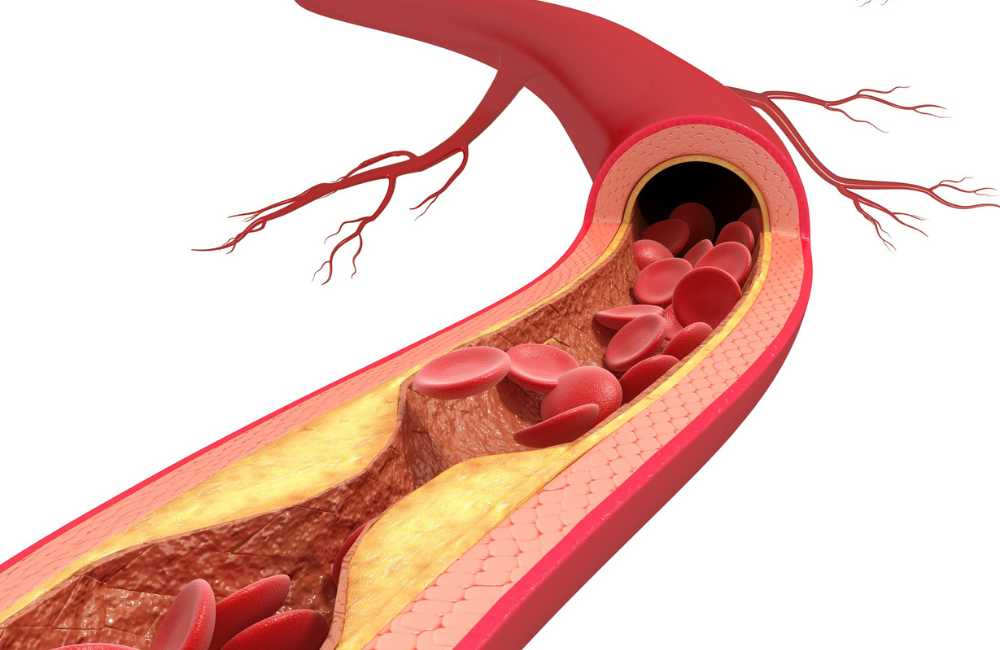
Coronary artery disease
Coronary artery disease is the cause of HF in two-thirds of patients with left ventricular (LV) systolic dysfunction. Measurable decreases in systolic function may be present for months or years before overt HF symptoms develop. Acute myocardial ischemia and myocardial infarction can result in sudden changes in systolic and diastolic ventricular function and acute HF with systemic congestion.
-
Other causes of cardiomyopathy
Viral infections, diabetes mellitus, and excessive alcohol intake have direct effects on the myocardium and can lead to cardiomyopathy and ventricular dysfunction. Diabetes is emerging as a significant causative factor for the development of HF.
-
Valvular disease
Significant valvular stenosis, regurgitation, or both, particularly in the mitral or aortic valves, are well-documented factors that contribute to ventricular. dysfunction, and are commonly seen in the elderly as a contributing factor for HF.
Symptoms of congestive heart failure
-
Shortness of breath (also called dyspnea)
Sudden onset breathlessness during activity most commonly, at rest, or while sleeping and wakes the patient up. This can come on while lying flat and may need to prop up the upper body and head on two pillows. The patient also complains of waking up tired or feeling anxious and restless.

-
Persistent coughing or wheezing
Coughing produces white or pink blood-tinged mucus.
-
The buildup of excess fluid in body tissues (oedema)
Swelling in the feet, ankles, legs or abdomen or weight gain. You may find that your shoes feel tight.
-
Tiredness, fatigue
Feeling of being tired all the time and having difficulty with everyday activities, such as shopping, climbing stairs, carrying shopping bags or walking.
-
Lack of appetite, nausea
a feeling of being full or sick to your stomach.
-
Confusion, impaired thinking
Memory loss and feelings of disorientation. A caregiver or relative may notice this first.
-
Increased heart rate
Heart palpitations, which feel like your heart is racing or throbbing.
Investigations
-
Radiological investigations
-
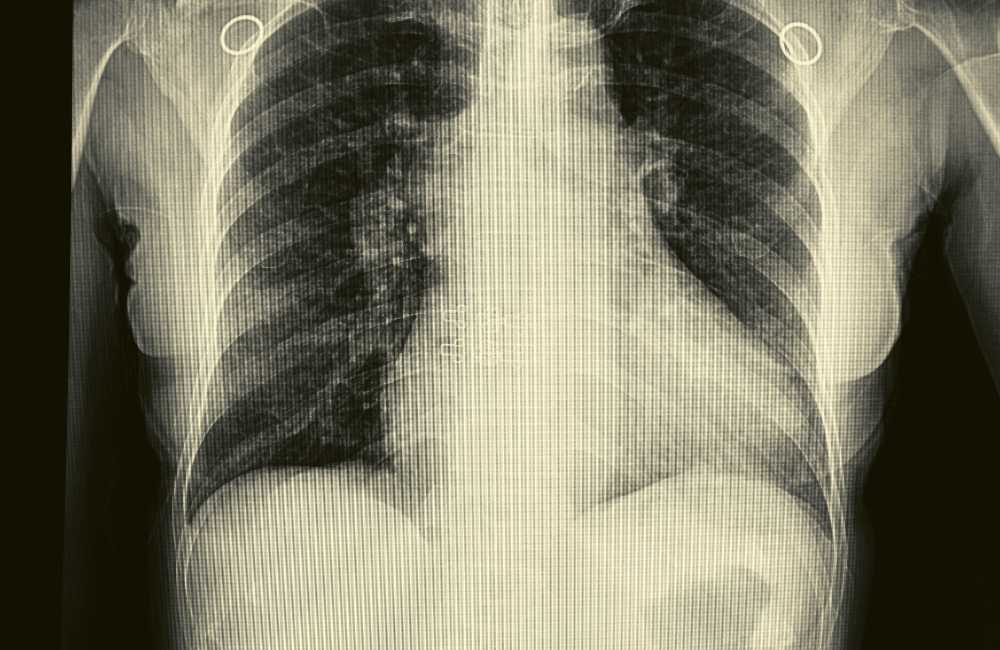
- Chest X-Ray
Findings in HF patients may include the following:
-
-
- Enlarged Heart (Cardiomegaly).
- Pulmonary oedema
-
-
- Electro- cardiogram (ECG or EKG)
ECG findings are not diagnostic, but an abnormal ECG, especially showing previous myocardial infarction, left ventricular hypertrophy, left bundle branch block, or tachyarrhythmia (e.g., rapid atrial fibrillation increases suspicion for HF and may help identify the cause. An entirely normal ECG is uncommon in chronic HF.
-
- Echo cardiograph
Can help evaluate chamber dimensions, valve function, left ventricular ejection fraction ( LVEF), wall motion abnormalities, left ventricular hypertrophy, diastolic function, pulmonary artery pressure, left ventricular and right ventricular filling pressures, Right ventricular function, and pericardial effusion. Intracardiac thrombi, tumours, calcifications within the heart valves, mitral annulus, and aortic wall abnormalities can be detected.
-
- Coronary angiography
This should be performed in HF patients who have angina or evidence of ischemia and be considered for revascularization if indicated.
-
- Cardiac MRI
This provides accurate images of cardiac structures and is becoming more widely available.
-
- Thoracic ultrasonography
This is a non-invasive method of detecting pulmonary congestion in patients with heart failure. Sonographic “comet tail artefact” on thoracic ultrasonography corresponds to the x-ray finding of Kerley B lines.
-
Laboratory testing in a patient with a new HF diagnosis
-
- Complete blood count (anaemia).
- Urinalysis.
- Electrolytes/urea/creatinine.
- Thyroid studies (T4, thyroid-stimulating hormone; hypothyroidism).
- Biomarker tests
B-type natriuretic peptide (BNP) is a hormone that is a marker of the severity and prognosis of heart failure. BNP is elevated in both systolic and diastolic HF. BNP can be helpful when the physician is unclear if the patient has dyspnea caused by HF or to other non-cardiac causes.
However, a normal BNP level does not exclude the diagnosis of heart failure, particularly in patients with HFpEF and/or obesity.
Diagnosing congestive heart failure
- History.
- Physical examination.
- Results of the investigations done.
Treatment for congestive heart failure
The heterogeneous nature of HF mandates an individualized approach to treatment but the primary goal is to diagnose and correct or treat the disorder that led to heart failure.
- Diet and lifestyle changes.
- Treatment of cause.
- Drug therapy.
- Sometimes device therapy (e.g., implantable cardio-vertercardioverter-defibrillator, cardiac resynchronization therapy, mechanical circulatory support)
- Sometimes-cardiac transplantation.
- Multidisciplinary care.
How is congestive heart failure prevented?
Avoiding the conditions that contribute to it or carefully managing the conditions if they develop prevents heart failure.
-
Stopping smoking
Smoking is a major factor in arterial damage that can cause heart failure. Stopping smoking or better still not starting. Also, secondhand smokers are not except.
-
Healthy diet
Foods containing little saturated fat, trans fat, sugar or sodium are discouraged. Smart eating is advised viz fruits and vegetables, low-fat dairy, lean protein such as chicken without the skin, and “good” fats such as those found in olive oil, fish and avocadoes.
-
Weight reduction
Lose weight if overweight. Along with diet, being physically active helps achieve this goal and is also great for the heart.
-
Dealing with comorbidities
Patients with other heart diseases or related conditions should closely follow the treatment program advised.
Conclusion
There’s no cure for heart failure and it worsens over time, so you need to be familiar with changes in your body. Some of these can be addressed with different medications.
Treatment aims to relieve symptoms and slow further damage. The exact plan depends on the stage and type of heart failure, underlying conditions and the individual patient.