Chest pain is one of the most common symptoms for which adults seek the care of a physician. It generally originates from one of the following organs in the chest viz:
- Heart.
- Lung.
- Oesophagus.
- From the components of the chest wall.
-
- Skin.
- Muscle.
- Bone.
- Occasionally, organs near the chest can cause chest pain. Such as:
-
- The gallbladder.
- Stomach.
- Pain in the chest may also be the result of “referred pain” from the neck or shoulder joint.
- Psychological.
Chest pains can be described by patients as dull, burning, pressure, tightness or squeezing depending on the cause and can be located in one or several areas (middle of the chest, upper or left chest, back, arms, jaw, neck, or the entire chest area).
Pain may also worsen with activity and improve with rest, and there may be other symptoms like sweating, feeling like throwing up rapid heart rate, and shortness of breath.
What is Chest Pain?
Chest pain (CP) is discomfort or pain that is experienced anywhere along the front of the body between the neck and the upper abdomen. The chest pain can be viz:
- Acute (less than 72 hours).
- Subacute (3 days to a month).
- Chronic (more than a month).
- Chronic with an acute exacerbation.
In the ER, chest pain is the second most common complaint comprising approximately 5% of all emergency room visits. In evaluating for chest pain, the provider should always consider life-threatening causes of chest pain e.g.
-
Acute coronary Syndrome (ACS)
A term used to describe a range of conditions associated with sudden, reduced blood flow to the heart.
-
- Coronary Artery Disease (CAD) – When Cholesterol builds up, narrows and blocks the blood vessels that carry blood to the heart.
-
- Heart attack (myocardial infarction) — when cell death results in damaged or destroyed heart tissue. Angina is chest pain or discomfort caused when the heart muscle doesn’t get enough oxygen-rich blood.
-
Coronary Artery Dissection
The coronary artery wall rips up, creates a bulge and blocks the artery. This causes pressure or pain in your chest, and it could lead to a heart attack.
-
Aortic Dissection
Occurs when a tear in the wall of the aorta, makes the layers of the wall come apart from each other thus resulting in a very excruciating pain that can come without warning. The patient feels like something is ripping and is often felt in the chest, back and between the shoulder blades.
-
Aortic Aneurysm
Here, the blood pushes against a weak part of the aorta’s wall thus making it bulge out. This weak spot can break open and cause severe pain in your chest or abdomen. If an aortic aneurysm ruptures, this becomes an emergency that requires immediate treatment.
-
Gastroesophageal Reflux Disease (GERD)
Acidic stomach content comes up into your oesophagus, causing a burning sensation or tightness (heartburn) in the epigastric region.
-
Musculoskeletal Causes
-
- Costochondritis
Inflammation of the cartilage that links most of the ribs to the breastbone. This can cause a sharp pain in your chest that gets worse during coughing or deep breathing.
Thus the precise definition of pain allows the list of possible causes to be narrowed and guides the comprehensive physical examination and choice of diagnostic tests (laboratory and imaging studies) to uncover potentially serious conditions
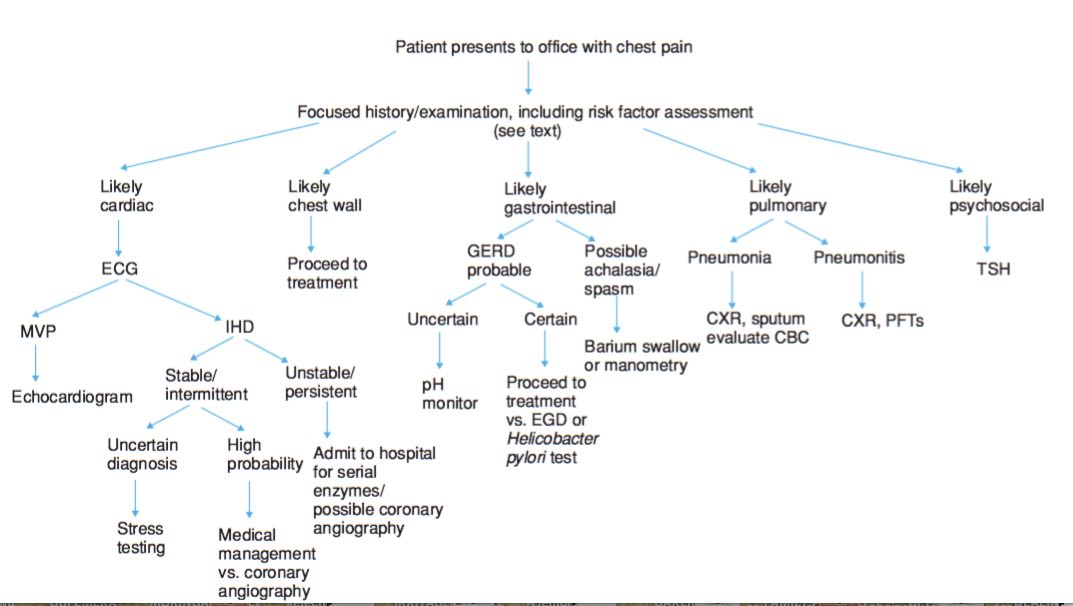
Chest Pain Evaluation
This starts with having a good understanding of the patient’s complaints, so a good history is very important.

The following are considered viz:
-
History
-
- Age of the patient
Patient age helps evaluate chest pain. Chest pain in children and adults less than 30 years is less likely to result from myocardial ischemia, although myocardial infarction can occur in people in their 20s. Musculoskeletal and pulmonary disorders are more common causes in these age groups.
-
- Onset
When did this pain start? And what brought it on? Exertion or when at rest?
-
- Location
Can the patient localize the pain with one finger or is it diffuse?
-
- Duration
The duration of pain can provide clues to the severity of the disorder. Long-standing pain (i.e., for weeks or months) is not a manifestation of a disorder that is immediately life-threatening. Such pain is often musculoskeletal in origin, although gastrointestinal origin or cancer should be considered, particularly in older patients.
Similarly, brief (less than 5 seconds), sharp, intermittent pains rarely result from serious disorders. Serious disorders typically manifest pain lasting minutes to hours, although episodes may be recurrent (e.g., unstable Angina may cause several bouts of pain over 1 or more days).
-
- Character
How is the pain?
-
- Aggravating/alleviating factors
What makes the pain worse? Or what makes the patient feel better? Angina pains are aggravated by physical or emotional stress. Nitroglycerin may relieve the pain of both myocardial ischemia and non-cardiac smooth muscle spasm (e.g., oesophagal or biliary disorders); its efficacy or lack thereof should not be used for diagnosis.
-
- Radiation
Does the pain radiates or moves to any other part of the body?
With angina, the pain often spreads to other areas of the upper body. This may include the neck, throat, lower jaw, teeth, or shoulders and arms. Sometimes, pain is felt in the wrists, fingers, or back (between the shoulder blades).
-
- Timing
When does the patient experience this pain? For how long does it stay on?
Angina pain tends to come on gradually and typically gets worse over several minutes.
-
- Associated phenomenon
- Fever.
- Excessive sweating (Diaphoresis).
- Cough.
- Dyspepsia.
- Shortness of breath.
- Nausea and vomiting.
- Oedema.
- Calf pain or swelling.
- Recent illness.
- Associated phenomenon
Chest pain associated with fever and cough is more likely to be of pulmonary cause.
-
Review of Systems
A review of systems should seek symptoms of the possible cause. If there is leg pain, swelling, or both, deep vein thrombosis (clotting in the extremity especially calf or thigh) could be a possibility and therefore possible pulmonary embolism while chronic weakness, malaise, and weight loss may suggest malignancy.
-
Past Medical / Drug History
Past medical/drug history that is documented is reviewed here, particularly cardiovascular and gastrointestinal (GI) disorders.
- Cardiac investigations or procedures.
- Risk of coronary artery disease (CAD) e.g., hypertension, raised cholesterol levels, diabetes, cerebrovascular disease, tobacco use).
- Pulmonary embolism (e.g., lower extremity injury, recent surgery, immobilization, known cancer, pregnancy should also be noted.
- Drug history should note the use of drugs that can trigger coronary artery spasmspasms (e.g., cocaine) or GI disease (particularly alcohol, and nonsteroidal anti-inflammatory drugs).
- Family history should note the history of myocardial infarction (particularly among 1st-degree relatives at an early age, i.e. more than 55 in men and more than 60 in women) and raised cholesterol levels.
-
Physical Examination
The physical examination is guided by clinical suspicion.
Red Flags for Chest Pain
Certain findings raise suspicion of a more serious cause of chest pain:
- Abnormal vital signs (fast and rapid heart rate, low pulse rate, fast breathing, low blood pressure)
- Signs of hypoperfusion (e.g. confusion, ashen colour, profuse sweating).
- Shortness of breath.
- Low oxygen saturation on pulse oximetry.
- Asymmetric breath sounds or pulses.
- New heart murmurs.
- Pulsus paradoxus > 10 mm Hg.
Investigations for Chest Pain
For patients with acute chest pain, immediate life threats must be ruled out.

The following can be done Viz:
- Pulse oximetry measures oxygen saturation.
- ECG or EKG at rest or exercise – records the heart’s electrical activity.
- Chest x-ray.
- Echocardiography (Cardiac Echo)
This can be particularly useful in identifying:
-
- Left ventricular or right ventricular dysfunction.
- Evidence of right ventricular pressure overload.
- Valvular pathology.
- Pericardial effusions.
- Signs of pericardial tamponade.
- CT- Cardiac angio.
- If symptoms suggest an acute coronary syndrome or if no other cause is clear (particularly in at-risk patients), cardiac enzymes like troponin levels are measured.
- If a pulmonary embolism (PE) is considered possible, D-dimer testing is done in low and intermediate-risk patients.
The likelihood of pulmonary embolism is affected by several clinical factors, which can be used to derive an approach to testing. Many of these factors are included in scoring systems that help determine the probability of PE such as:
-
- The Wells Scoring System.
- The Revised Geneva Scoring System
- The Pulmonary Embolism Rule Out Criteria.
Expeditious evaluation is essential because if myocardial infarction or other acute coronary syndrome is present, the patient should be considered for urgent heart catheterization (when available). Immediate catheterization is indicated in patients with ST-elevation on ECG or non–ST-segment elevation myocardial infarction (NSTEMI) causing hypotension, ventricular arrhythmias, or persistent chest pain despite optimal medical management.
Some abnormal findings on these tests can confirm a diagnosis while other abnormalities suggest the need to pursue further investigation. However, in acute coronary syndromes, ECG may not change for several hours or sometimes not at all, and in pulmonary embolism, oxygenation may be normal. Thus, other studies may need to be obtained based on findings from the history and physical examination.
Because a single normal set of cardiac markers does not rule out a cardiac cause, patients whose symptoms suggest an acute coronary syndrome should have a serial measurement of the cardiac marker troponin and ECGs.
For Acute coronary syndrome, drug treatment is begun while awaiting the results of the 2nd troponin level unless there is a clear
Contraindication
Troponin will be elevated in acute coronary syndromes except in unstable angina, and often in other disorders that damage the myocardium (e.g. myocarditis, pericarditis and aortic dissection)
Creatine kinase (CK) may be elevated due to damage to any muscle tissue, but creatine kinase-MB isoenzyme (CK-MB) elevation is specific to damage to the heart muscles (myocardium). However, troponin is the standard marker of cardiac muscle injury.
Advances in high-sensitivity troponin assays allow for more rapid serial evaluation of a possible acute coronary syndrome. With improved negative predictive value, high sensitivity high-sensitivity troponin also has the potential to decrease the necessity of further testing in patients with negative biomarkers and has been demonstrated to allow patients to be discharged more quickly.
Recent guidelines recommend using normal troponin levels and negative coronary CT scanning as a reliable strategy to exclude acute coronary syndrome in patients with chest pain and no red flags.
ST-segment abnormality on the ECG may be nonspecific or due to antecedent disorders, so comparison with previous ECGs is important. Some clinicians follow initial testing with a stress ECG or a stress-imaging test.
In patients with chronic chest pain, immediate threats to life are unlikely. Most clinicians initially obtain a chest x-ray and do other tests based on symptoms and signs.
Evaluation Flow Chart for Chest Pain
When Do I Get Worried?
If you have recent onset chest pain which makes the chest feel tight or heavy, that lasts longer than fifteen minutes and doesn’t go away when after a rest or medication or spreads to the arms, neck or jaw and back or starts with shortness of breath, sweating and feeling or being sick, please get immediate medical help.
Treatment for Chest Pain
Specifically identified disorders are treated. If the cause of chest pain is uncertain, the patient should be admitted to the hospital for observation and cardiac monitoring and more extensive evaluation.
Pain management is with acetaminophen or with opioid analgesics as needed pending a diagnosis. If pulmonary embolism is highly likely, antithrombin drugs should be given while the diagnosis is pursued because the second embolus in a patient who is not receiving anticoagulants may be fatal.
Conclusion
Chest pain is a serious symptom. If you think yours might be due to a heart attack, take action right away. Get Medical help immediately. Do not attempt to drive yourself to the hospital and do not ask someone else to drive you.
Calling for an ambulance is safer than driving because the Paramedical medical staff are trained to initiate treatment even when being transported to the Hospital. ..

