Breast cancer is the second most common cancer in women after skin cancer. It is most often found in women, Men can also get it too. It is found out that 1 out of every 100 breast cancers diagnosed in the United States is a man. In Men, manifestations, diagnosis, and management are the same, although, in men, it tends to present at a late stage.
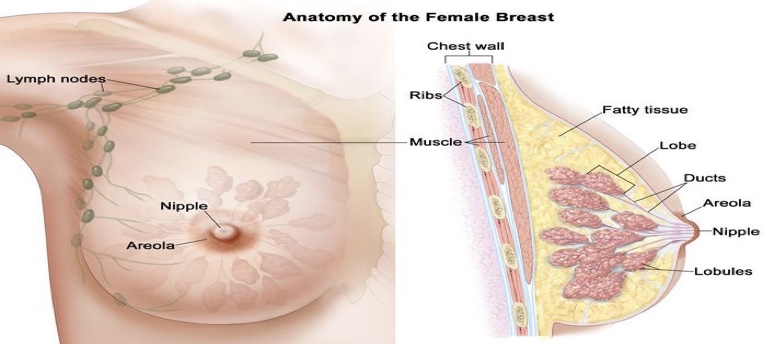
The female breast is made up of lobes and ducts. Each breast has 15-20 lobes. Each lobe has many smaller sections called lobules. Lobules end in dozens of tiny bulbs that make milk. Thin tubes called ducts link the lobes, lobules and bulbs.
Each breast also has blood vessels and lymph vessels (which carry an almost colourless, watery fluid called lymph between lymph nodes). Lymph nodes are small, bean-shaped structures found throughout the body that filter lymph and store white blood cells that help fight infection and disease. Groups of lymph nodes are found near the breast under the arm, above the collarbone and in the chest.
The most common type of breast cancer is ductal carcinoma, which begins in the cells of the ducts. Cancer that begins in the lobes or lobules is called lobular carcinoma and is more often found in both breasts than are other types.
Inflammatory breast cancer is an uncommon type of breast cancer in which the breast is warm, red and swollen.
Therefore when we say “breast cancer,” we mean cancers that form in milk ducts or lobules (also called epithelial tumours -that is they develop from cells lining ducts or lobules) Cancers can also form in other parts of the breast, but these types of cancers are less common. They are also called non-epithelial cancers of the supporting stroma and they include:
- Angiosarcoma
This rare type of cancer begins in the cells of the lining of blood or lymph vessels.
- Primary stromal sarcomas of the breast
A rare entity that occurs in less than 1% of women with breast malignancy.
- Phyllodes tumour
Phyllodes are rare tumours that start in the connective tissue of the breasts, they’re usually benign (non-cancerous), but they can be malignant (cancerous) in some cases.
Cancer invades locally and spreads through the regional lymph nodes, bloodstream, or both. Metastatic breast cancer may affect almost any organ in the body—most commonly, the lungs, liver, bone, brain, and skin.
Most skin metastases occur near the site of breast surgery. Scalp metastases are uncommon.
What is breast cancer?
Breast cancer originates in the breast tissue. It occurs when breast cells mutate (change) and grow out of control, creating a mass of tissue (tumour). Like other cancers, breast cancer can invade and grow into the tissue surrounding the breast.
It can also travel to other parts of the body and form new tumours. When this happens, it’s called metastasis.
Types of breast cancer
Breast cancers are divided into carcinoma in situ and invasive cancer.
-
Carcinoma in situ
This is the proliferation of cancer cells within the ducts or lobules without invasion of stromal tissue. There are 2 types viz:
-
- Ductal carcinoma in situ (DCIS)
About 85% of carcinoma in situ are this type. DCIS is usually detected only by mammography. It may involve a small or wide area of the breast; if a wide area is involved, microscopic invasive foci may develop over time.
-
- Lobular carcinoma in situ (LCIS)
LCIS is often multifocal and bilateral. There are 2 types viz: Classic and Pleomorphic.
-
-
- Classic LCIS
-
This non-palpable lesion detected by biopsy is usually non-malignant but increases the risk of developing invasive carcinoma in either breast. It is rarely visualized with mammography.
-
-
- Pleomorphic LCIS behaves more like DCIS
-
It should be excised to negative margins.
-
Invasive carcinoma
This is primarily an adenocarcinoma( cancer that develops in the glands that line organs) and accounts for about 80% of the infiltrating ductal type while the remaining 20 % of cases are infiltrating lobular.
Rare types include
-
- Medullary.
- Mucinous.
Mucinous carcinoma tends to develop in older women and are slow growing.
-
- Metaplastic.
- Tubular carcinomas.
Women with most of these rare types of breast cancer have a much better prognosis than women with other types of invasive breast cancer. Also note, there is what is called inflammatory breast cancer and Triple Negative Breast cancer.
The inflammatory breast cancers
This is a fast-growing, particularly aggressive, and often fatal cancer. In this situation, cancer cells block the lymphatic vessels in the skin of the breast and as a result, the breast appears inflamed, and the skin appears thickened, resembling orange peel (peau d’orange). Usually, in inflammatory breast cancers, no masses are felt in the breast itself.

Triple Negative Breast cancer (TNBC) namely, estrogen receptor, progesterone receptor, and HER2/neu negative.
TNBC is one of the most challenging breast cancers to treat. This makes up about 15% of all breast cancer cases, it’s called triple negative because it doesn’t have three of the markers associated with other types. This makes prognosis and treatment difficult.
What are the risk factors of breast cancer?
Factors that may affect breast cancer risk include the following:
- Age
The strongest risk factor is age. The median age at diagnosis is about 60 years.
- Family history
Having a 1st-degree relative (mother, sister, daughter) with breast cancer doubles or triples the risk of developing cancer, although, breast cancer in more distant relatives increases the risk only slightly. When ≥ 2 1st-degree relatives have breast cancer, the risk may be 5 to 6 times higher.
- Breast cancer gene mutation
About 5 to 10% of women with breast cancer carry a mutation in one of the two known breast cancer genes, BRCA2. The risk of developing breast cancer by age 80 is about 72% with a BRCA2 mutation.
Women without a family history of breast cancer in at least two 1st-degree relatives are unlikely to carry this mutation. BRCA1 or estrogen-receptor modulators in men reduce the risk of developing breast cancer.
- Hormone receptors
-
- Estrogen and progesterone receptors
Some breast cancer cells have receptors for the hormones estrogen or progesterone. These cells are hormone receptor-positive and they need estrogen or progesterone to grow.
About two thirds of postmenopausal patients with cancer are estrogen receptor–positive (ER+). Incidence of ER+ tumors is lower among premenopausal patients.
-
- Human epidermal growth factor receptor 2 (HER2)
Also called HER2/neu or ErbB2), human EGF receptor 2and, human epidermal growth factor receptor 2. A protein is involved in normal cell growth. HER2 may be made in larger than normal amounts by some type of cancer cells, including breast, ovarian, bladder, pancreatic, stomach and oesophagal cancers.
This may cause cancer cells to grow more quickly and spread to other parts of the body. Checking the amount of HER2 on some types of cancer cells may help plan treatment.
Its presence correlates with a poorer prognosis at any given stage of cancer. In about 20% of patients with breast cancer, HER2 receptors are over-expressed.
Drugs that block these receptors are part of standard treatment for these patients.
- Radiation therapy
Exposure to radiation therapy before age 30 increases the risk of developing breast cancer.Radiation therapy for Hodgkin lymphoma quadruples the risk of breast cancer over the next 20 to 30 years.
- Diet
Diet may contribute to the development or growth of breast cancers, but conclusive evidence about the effect of a particular diet (e.g., one high in fats) is lacking. Obese postmenopausal women are at increased risk, but there is no evidence that dietary modification reduces risk. For obese women who are menstruating later than normal, risk may be decreased.
- Lifestyle factors
Smoking and alcohol may contribute to a higher risk of breast cancer.
In epidemiologic studies, alcohol intake is associated with a higher risk of breast cancer however, causality is difficult to establish.
- Hormone replacement therapy
People who use hormone replacement therapy (HRT) have a higher risk of being diagnosed with breast cancer.
Early signs/symptoms of breast cancer
Breast cancer symptoms can vary from person to person. Possible signs of breast cancer include:
- A change in the size, shape or contour of the breast.
- A mass or lump, which may feel as small as a pea.
- A lump or thickening in or near the breast or in the underarm that persists through the menstrual cycle.
- A change in the look or feel of the skin over the breast or nipple (dimpled, puckered, scaly or inflamed).
- Redness of the skin over the breast or nipple.
- An area that’s distinctly different from any other area on either breast.
- A marble-like hardened area under the skin.
- A blood-stained or clear fluid discharge from the nipple.
- Some people may not notice any signs of breast cancer at all. That’s why routine mammograms are so important.
Investigations for breast cancer
- Chest x-ray.
- Complete blood count (CBC).
- Liver tests.
- Measurement of serum calcium levels should be done to check for metastatic disease.
- An oncologist should determine whether to measure serum carcinoembryonic antigen (CEA), cancer antigen (CA) 15-3, or CA 27-29 and whether bone scanning should be done.
- Mammogram
These special X-ray images can detect changes or abnormal growths in the breast. A mammogram is commonly used in breast cancer prevention.
-
- Breast tomosynthesis (3-dimensional mammography) – done with digital mammography
This increases the rate of cancer detection slightly and decreases the rate of recall imaging. This test is helpful for women with dense breast tissue. However, the test exposes women to almost twice as much radiation as traditional mammography.
Although mammography uses low doses of radiation, radiation exposure has cumulative effects on cancer risk. When radiologic screening is started at a young age, the risk of cancer is increased.

- Ultrasonography
This test uses sound waves to take pictures of the tissues inside the breast. It’s used to help diagnose breast lumps or abnormalities.
- Positron emission tomography (PET) scanning.
PET scan uses special dyes to highlight suspicious areas. During this test, the healthcare provider injects a special dye into the veins and takes images with the scanner.
- CT Abdomen
- Magnetic resonance imaging (MRI)
This test uses magnets and radio waves to produce clear, detailed images of the structures inside of your breast.
- Gene test for Mutation
Cells from blood or saliva should be tested for inherited gene mutations that predispose to breast cancer when:
-
- Breast cancer develops at age less than 45 years of age.
- The cancer does not have estrogen or progesterone receptors or overexpression of HER2 protein (triple negative breast cancer).
- Breast and ovarian cancers occur in the same patient.
- Patients have lobular breast cancer plus a personal or family history of diffuse gastric cancer.
- Their family history includes multiple cases of early-onset breast cancer.
- Family history of multiple cases of ovarian, pancreatic, or prostate cancer.
- Patients have an Ashkenazi Jewish heritage.
- Patient is male and their family history includes any cases of male breast cancer.
Some experts have recommended that genetic testing be offered to all patients with breast cancer.
Diagnosis of breast cancer
- History
-
- Personal History.
- Family History.
- Gynaecology History.
- Clinical Breast Examination (CBE)
Breast examination by health care practitioners
- Results of the screening and investigations listed above.
- Biopsy
Percutaneous core needle biopsy is preferred to surgical biopsy. A core biopsy can be done guided by imaging or palpation (freehand).
Staging of breast cancers
In breast cancer, stage is based on the size and location of the primary tumour, the spread of cancer to nearby lymph nodes or other parts of the body, tumor grade and whether certain biomarkers are present.
To plan for the best treatment and understand the prognosis, it is important to know the breast cancer stage. There are 3 types of breast cancer stage groups.
-
Clinical prognostic stage
This is assigned to all patients regardless of the type of therapy used.
The clinical prognostic stage is described by the TNM system, tumour grade and biomarker status(ER, PR, HER2). Also, mammography or ultrasound is used to check the lymph nodes for signs of cancer.
-
Pathological prognostic stage
This is used for patients who have had surgery as their first treatment. The pathological prognostic stage is based on all clinical information, biomarker status, and laboratory test results from the breast tissue and lymph node removed during surgery.
-
Anatomic stage
This is based on the size and the spread of cancers described by the TNM system. The Anatomic stage is used in parts of the world where biomarker testing is not available.
Treatment for breast cancer
After cancer is diagnosed, a multidisciplinary evaluation is usually done to plan further testing and treatment. The core multidisciplinary team typically includes a breast surgical oncologist, medical oncologist, and radiation oncologist.
A positive biopsy specimen should be analyzed for estrogen and progesterone receptors and for HER2 protein. There are several breast cancer treatment options viz
-
Surgery
This involves removing the cancerous portions of the breast and an area of normal tissue surrounding it. They include:
-
- Lumpectomy (Partial mastectomy)
The tumour and a small margin of healthy tissue around it are removed. Also some of the lymph nodes in the breast or under the arm are removed for evaluation. People who have a lumpectomy often have radiation therapy in the weeks following the procedure.
-
- Mastectomy
Removal of the entire breast. In some cases, doctors can perform a nipple-sparing mastectomy to preserve the nipple and areola (the dark skin around your nipple).

-
-
- Radical mastectomy.
-
This procedure is performed when the breast cancer has spread to the chest wall muscles. During this surgery, the surgeon removes the entire breast, the nipple, underarm lymph nodes and chest wall muscles.
-
-
- Modified radical mastectomy.
-
During this procedure, the entire breast, the nipples, and nearby lymph nodes in the underarm area are removed, but the chest muscles are left intact.
-
-
- Contralateral prophylactic mastectomy.
-
A contralateral prophylactic mastectomy is an option for some women with breast cancer (e.g., those with a genetic mutation conferring a high risk of breast cancer). Also in women with lobular carcinoma in situ in one breast, invasive cancer is equally likely to develop in the second breast. Thus, the only way to eliminate the risk of breast cancer for these women is bilateral mastectomy. Some women, particularly those who are at high risk of developing invasive breast cancer, choose this option.
-
- Lymph node evaluation
During both mastectomy and breast-conserving surgery, axillary lymph nodes are typically evaluated. Methods include viz
-
-
- Sentinel node biopsy SLNB)
-
For SLNB, blue dye and/or radioactive colloid are injected around the breast, and a gamma probe is used to locate the nodes the tracer drains into. If dye is used, direct inspection is done. Because these nodes are the first to receive the tracers, they are considered the most likely to receive any metastatic cells and are thus called sentinel nodes.
If any of the sentinel nodes contain cancer cells, axillary lymph node dissection may be necessary.
-
-
- Axillary lymph node dissection. (AND)
-
If multiple lymph nodes are involved in the cancer, an axillary lymph node dissection may be done to remove them. ALND is a fairly extensive procedure that involves the removal of as many axillary nodes as possible; adverse effects, particularly lymphedema, are common.
-
Chemotherapy
Chemotherapy or endocrine therapy delay prevent recurrence in almost all patients and prolong survival in some. However, studies have shown that chemotherapy is not necessary for many small (< 0.5 to 1 cm) tumors with no lymph node involvement (particularly in postmenopausal patients) because the prognosis is already excellent.
-
Radiation therapy
Radiation therapy after breast-conserving surgery significantly reduces the incidence of local recurrence in the breast and in regional lymph nodes and may improve overall survival.
-
Hormone therapy
Endocrine therapy is preferred over chemotherapy for patients with any of the following:
-
- Estrogen receptor positive status (ER+ tumours).
- A disease-free interval of more than 2 years.
- Disease that is not immediately life-threatening.
-
Targeted drug therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy does.
-
Immunotherapy (biological therapy)
This is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in the laboratory are used to boost, direct or restore the body’s natural defenses against cancer. This type of cancer treatment is an example of biological therapy.
-
Reconstructive procedures
Reconstructive procedures include the following:
-
- Prosthetic reconstruction:
Placement of a silicone or saline implant, sometimes after a tissue expander is used.
-
- Autologous reconstruction:
Muscle flap transfer (using muscles from a different part of the body to reconstruct the breast). Breast reconstruction can be done during the initial mastectomy or breast-conserving surgery or later as a separate procedure.
-
Fertility preservation
Patients with breast cancer should not become pregnant while being treated for breast cancer. However, all patients who wish to preserve fertility should be referred to a reproductive endocrinologist to discuss fertility preservation before systemic therapy is initiated.
What’s right for one depends on many factors, including the location and size of the tumor, the results of the lab tests and whether the cancer has spread to other parts of the body. The healthcare provider will tailor the treatment plan according to the unique needs of individuals. It’s common to receive a combination of different treatments, too.
Prognosis
Long-term prognosis depends on the tumor stage. Nodal status (including the number and location of nodes) correlates with disease-free and overall survival better than any other prognostic factor.
A poorer prognosis is associated with the following other factors:
- Young age
Prognosis appears worse for patients diagnosed with breast cancer during their 20s and 30s than for patients diagnosed during middle age.
- Race
Black women diagnosed at a younger age compared with white women (median 59 versus 63 years) are more likely to have the triple-negative disease.
- Larger primary tumour
Larger tumors are more likely to be node-positive, but they also confer a worse prognosis independent of nodal status.
- High-grade tumour
Patients with poorly differentiated tumors have a worse prognosis.
- Absence of estrogen and progesterone receptors
Patients with ER+ tumours have a somewhat better prognosis and are more likely to benefit from endocrine therapy. Also Patients with progesterone receptors on a tumour may have a better prognosis while Patients with both estrogen and progesterone receptors on a tumor may have a better prognosis than those who have only one of these receptors, but this benefit is not clear.
- Presence of HER2 protein
With either gene mutation, the risk of a 2nd cancer in the remaining breast tissue is increased (to perhaps as high as 40%).
Side effects of breast cancer treatment
Some side effects start with the commencement of treatment and may continue or appear months or years after treatment has ended. These are called late effects
Late effects of radiation therapy are not common, but may include:
- Lung inflammation after the radiation therapy to the breast, especially when chemotherapy is given at the same time.
- Arm Lymphedema especially when radiation therapy is given after lymph node dissection.
- In women younger than 45 years who receive radiation therapy to the chest wall after mastectomy may be at a higher risk of developing breast cancer in the other breast.
- Late effects of chemotherapy depend on the drugs used, but may include:
-
- Heart failure
- Blood clot
- Premature menopause
- Second cancer such as leukaemia.
- Late effects of targeted therapy may include:
-
- Heart problems such as heart failure.
Conclusion
While one can’t prevent breast cancer altogether, certain things can be done to reduce the risk of discovering breast cancer at an advanced stage. For example:
- Getting routine mammograms
Most cancer societies recommend having a baseline mammogram at age 35 and a screening mammogram every year after age 40.
- Breast self-examination (BSE) every month after age 20
This makes one familiar with the breast contours and feels of the breasts and thus making one more alert to changes.
- Clinical breast examination (CBE)
Having one’s breasts examined by a healthcare provider at least once every three years after age 20, and every year after age 40. Clinical breast exams can detect lumps that mammograms may not find.

