Bell’s palsy can only be understood if we review the anatomy of the 7th cranial nerve, the facial nerve, its course, functions and the clinical correlations. The nerve has 2 pathways viz. Within the brain (Intracranial) and outside the brain (Extra cranial).
Intracranial
The nerve arises in the area of the mid-brain, called the pons. It begins with 2 roots namely:
- A large motor root.
- A small sensory root.
They travel through the internal ear meatus where they are in close proximity to the middle ear; from here they enter the facial canal. Here, three important events occur:
- The 2 roots fuse to form the facial nerve.
- They form a collection of nerve bodies called a ganglion.
- Gives out nerve supplies to the mucus gland and lacrimal gland, to the middle ear bone and a special sensory nerve to the anterior 2/3 of the tongue and also a supply to the submandibular /sublingual glands.(mostly parasympathetic)
Thereafter, the nerve exits the cranium
Extracranial
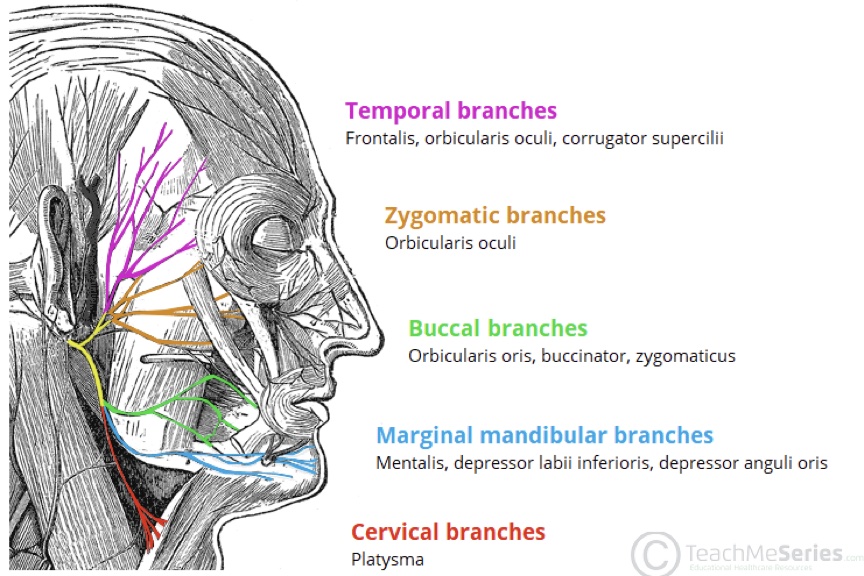
After exiting the brain, the nerve moves into the parotid gland and divides into 5 branches. These branches are responsible for the muscles of facial expressions. See a picture of the innervations in colour.
So basically, the facial nerve does the following:
- Controls the muscles that make facial expressions.
- Controls muscle in your inner ear that moderates the loudness of sound.
- Helps make tears.
- Sends information about tastes from the tongue to the brain.
What is Bell’s Palsy?
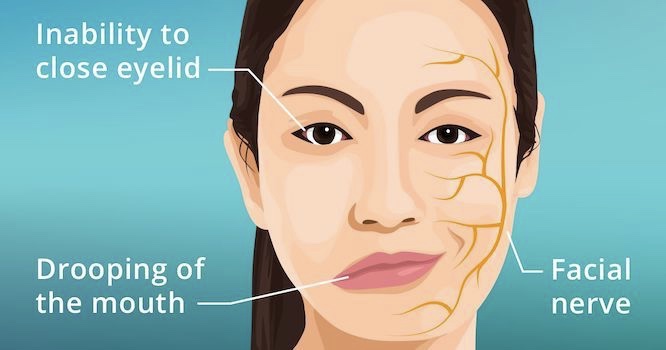
Bell’s palsy, also called facial nerve paralysis, is a sudden one-sided peripheral facial nerve palsy. It is the most common cause of one-sided facial paralysis and the most common neurologic disorder of the cranial nerves (see the image above). In the great majority of cases, it gradually resolves over time.
It can happen to anyone at any age. However, it occurs most often in pregnant women, and people who have diabetes, influenza, a cold, or another upper respiratory ailment. It affects men and women equally. It is less common before age 15 or after age 60.
Causes of Bell’s Palsy
The mechanism for Bell’s palsy is presumably swelling of the facial nerve due to an immune or viral disorder. Current evidence suggests common viral implicated as:
- Herpes Simplex Infection (most common)
- Herpes Zoster (possibly the second most common)
- Coxsackievirus, Cytomegalovirus, and the Epstein –Bar, Mumps, Rubella and Influenza B viruses. The swollen nerve is maximally compressed as it passes through the facial canal resulting in ischemia and paresis.
Bell’s Palsy Symptoms
These are the most common symptoms of Bell’s palsy:
- Disordered movement of the muscles that control facial expressions, such as smiling, squinting, blinking, or closing the eyelid.
- Loss of feeling in the face.
- Headache.
- Tearing.
- Drooling.
- Loss of the sense of taste on the front two-thirds of the tongue.
- Hypersensitivity to sound in the affected ear (hyperacusis).
- Inability to close the eye on the affected side of the face.
Diagnosis of Bell’s Palsy
Bell’s palsy is diagnosed from symptoms and clinical evaluation. There are no specific tests used to diagnose Bell’s palsy. However, some tests will be ordered to rule out other conditions that can cause similar symptoms and to determine the extent of nerve involvement or damage. These tests may include:
- Electromyography (EMG) to determine the extent of the nerve involvement.
- Blood tests to determine if another condition such as diabetes or Lyme disease is present.
- Chest x-ray or CT and serum angiotensin-converting enzyme (ACE) levels to check for sarcoidosis(a disease that is characterized by the growth of tiny collections of inflammatory cells).
- Magnetic resonance imaging (MRI) or computed tomography (CT) to determine if there is a structural cause for your symptoms.
Usually, clinicians can also distinguish Bell’s palsy from other disorders that cause peripheral facial nerve palsies based on their characteristic symptoms and signs; these disorders include the following:
- Herpes Zoster Oticus (geniculate herpes, Ramsay Hunt syndrome)
- Middle ear infections.
- Sarcoidosis.
- Lyme disease.
- Petrous bone fractures.
- Petrous bone fractures.
- Carcinomatous or leukemic nerve invasion.
Also, the other disorders that cause peripheral facial nerve palsy typically develop more slowly than idiopathic facial nerve palsy. Thus, if patients have any other neurologic symptoms or signs or if symptoms developed gradually, MRI should be done.
The Outcome of Bell’s Palsy
The extent of nerve damage determines the outcome. If some function remains, full recovery typically occurs within several months. The likelihood of complete recovery after total paralysis is 90% if nerve branches in the face retain normal excitability to supramaximal electrical stimulation and are only about 20% if electrical excitability is absent.

Bell’s Palsy Treatment
-
Protection for the Cornea
Corneal drying must be prevented by frequent use of natural tears, isotonic saline, or methylcellulose drops and by intermittent use of tape or a patch to help close the eye, particularly during sleep.
-
Corticosteroids Therapy
Help to reduce inflammation. Corticosteroids, if begun within 48 hours after onset, resulting in faster and more complete recovery. Prednisone 60 to 80 mg orally once a day is given for 1 week then decreased gradually over the 2nd week.
-
- Analgesics or moist heat to relieve pain.
- Physical therapy stimulates the facial nerve.
-
Anti-Viral Therapy
Antiviral drugs effective against herpes simplex virus:
-
- Valacyclovir 1 g orally 3 times a day for 7 to 10 days,
- Famciclovir 500 mg orally 3 times a day for 5 to 10 days,
- Acyclovir 400 mg orally 5 times a day for 10 days) has been prescribed.
But recent data suggest that antiviral drugs provide no benefit.
Conclusion
Bell’s palsy usually resolves in time and causes no long-term complications. It is important, however, to take medicines as directed. It is also crucial that you protect the affected eye from drying. The use of eye drops during the day and ointment at bedtime can protect the cornea from scratching.

