Bariatric surgeries or metabolic surgeries are the effective surgical management of obesity that can maintain weight loss. They also decrease obesity-associated co- morbid conditions. Obesity is related to the development of co-morbidities such as:
- Type II diabetes.
- Heart disease.
- Hypertension.
- Sleep apnea.
- Different orthopaedic disabilities.
Common Bariatric Surgeries
- Gastric Sleeve (also called Sleeve gastrectomy.
- Roux en-Y gastric bypass.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
- Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
Today’s metabolic /bariatric operations are performed with small incisions using minimally invasive surgical techniques (laparoscopic and robotic surgery).
These advancements allow patients to have a better overall experience with less pain, fewer complications, shorter hospital stays and a faster recovery. These operations are extremely safe, with low complication rates.
-
Gastric Sleeve (also called Sleeve Gastrectomy)
In the gastric sleeve, a soft plastic tube (called the Bougie) is inserted through the mouth to the oesophagus under endoscopy guidance to outline and form the new stomach. This helps the surgeon guide the cutter and places the stapler that holds the new stomach.
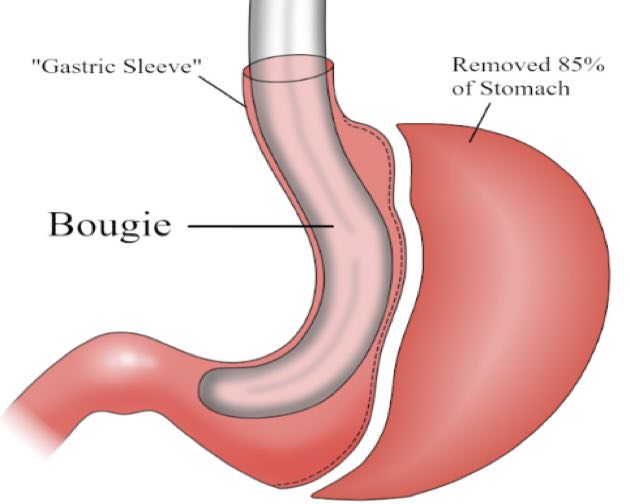
In gastric sleeve (sleeve gastrectomy), 80-85% of the stomach is cut along the great curvature and completely removed from the body, whereas, in the endoscopic sleeve gastrectroplasty, 70-80% of the stomach is isolated from the rest of the stomach by sewing it along the great curvature.
-
Roux en-Y Gastric Bypass
The Roux-en-Y gastric bypass (RYGB) is a two-step surgery. Firstly, a small pouch is created in the stomach with staples, thus leaving a larger part of the stomach separated from the pouch but not removed. The second step of this procedure involves dividing the small intestine just below the duodenum.
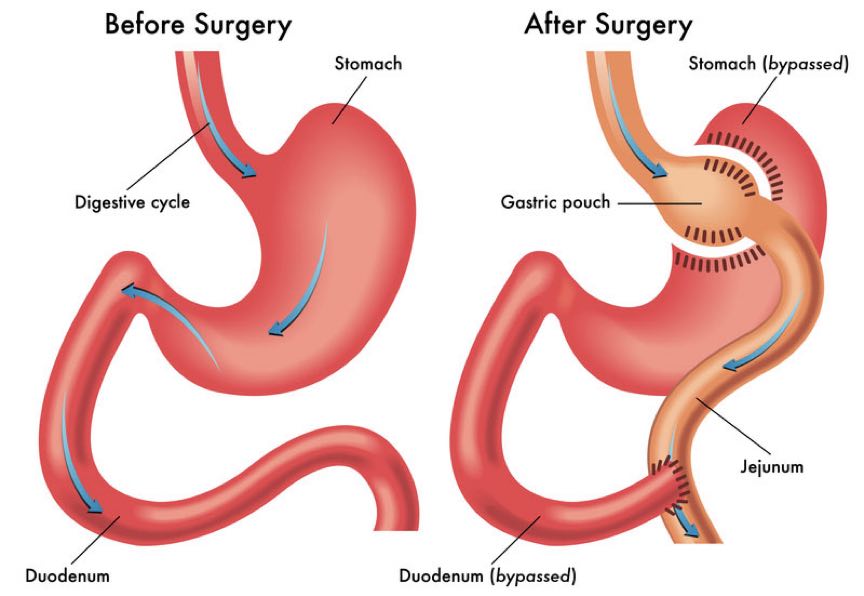
Thereafter, the jejunum is brought up and is connected to the newly created pouch while the duodenum is reconnected to the new intestinal limb giving the intestine thus forming the Y shape for which the procedure is named.
-
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
This is the traditional duodenal switch done as a 2-stage procedure:
- The first part of the surgery is a gastric sleeve.
- In the second part of the surgery, the duodenum is divided about 3cm after the pylorus, thus preserving the pylorus, next, the small bowel is divided 10 feet from the last part of the small intestine and then attached to the new stomach
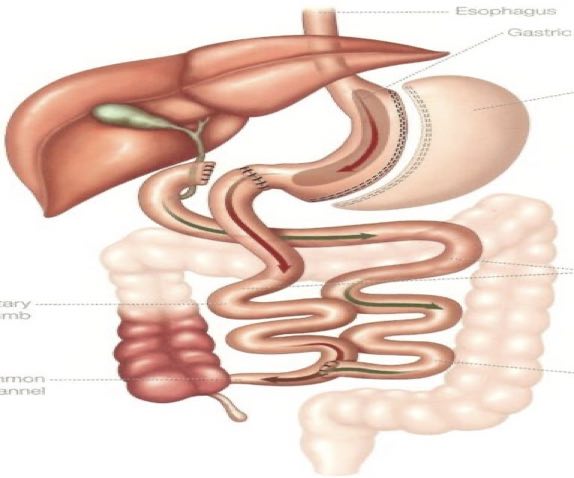 The remaining intestine is reconnected back to itself approximately 5 feet from the entrance into the large intestine (ileo-caecal junction).
The remaining intestine is reconnected back to itself approximately 5 feet from the entrance into the large intestine (ileo-caecal junction).
-
Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
Just like the traditional BDP/DS it’s a two-stage procedure. The first part is the gastric sleeve. In the second part, the first part of the small intestine is divided just after the stomach.
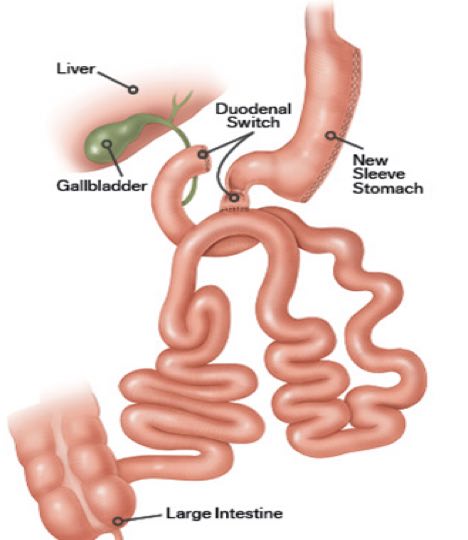
A loop of the intestine is measured several feet from its end and is then connected to the stomach. This is the only intestinal connection performed in this procedure.
Comparing Different Bariatric Surgeries
| S/N | Items | Sleeve gastrectomy | Roux en-Y gastric bypass | Biliopancreatic Diversion with Duodenal Switch (BPD/DS) | Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S). |
| 1 | Irreversibility | Irreversible | Reversible | Reversible | Reversible |
| 2 | Remission of obesity-associated conditions | Improvement of obesity-related conditions. | Effective for the remission of obesity-associated conditions. | Effective for the remission of obesity-associated conditions. | SADI is particularly beneficial for diabetic patients and has the highest resolution in type 2 diabetes. |
| 3 | Complexity | Not complex | Technically more complex when compared to sleeve gastrectomy | More complex surgery requiring more operative time | Simpler and faster to perform (one intestinal connection) than gastric bypass or BPD-DS. |
| 4 | Vitamin and mineral deficiencies | No Malabsorption | More vitamin and mineral deficiencies than sleeve gastrectomy or gastric banding | Highest malabsorption and greater possibility of vitamin and micronutrient deficiencies. Patients may have to take daily nutritional supplements for life. | Vitamins and minerals are not absorbed. |
| 5 | Risk of developing ulcers | There is a risk of developing ulcers, especially with NSAID or tobacco use | There is a risk of developing ulcers, especially with NSAID or tobacco use | The overall risk for Marginal ulcer is low, about 1% per patient-year | Does not increase ulcer risk in patients. |
| 6 | Dumping syndrome | Doesn’t cause dumping | but May cause dumping syndrome in about 85% of the cases. | Rarely causes dumping | Minimal risk of dumping syndrome. |
| 7 | Improving weight loss | Effective weight loss. | Reliable and long-lasting weight loss | Among the best results for improving obesity | An excellent option for a patient who already had a sleeve gastrectomy and is seeking further weight loss |
| 8 | Complications early after surgery | Less than 2% of major complication rate. | There is a risk of small bowel complications and obstruction | This is one of the most complicated and riskiest weight loss surgeries. | Reduced complications. |
| 9 | Treatment of DM | Lower rates of diabetic remission are noted. | Effective for the remission of type 2 diabetes. | Most effective procedure for the treatment of type 2 diabetes. | Highly effective for long-term remission of type 2 diabetes |
| 10 | Reflux and Heart Burns | Increased risk of reflux and oesophagal cancers if untreated ‘silent’ reflux continues. | The operation helps patients with reflux (heartburn) to improve quickly. | Reflux and heartburn can develop or get worse | Potential to worsen or develop new-onset reflux. |
| 11 | Diarrhoea | Many people experience diarrhoea after gastric sleeve surgery. | During the first weeks after the surgery, because more liquid foods are eaten, This problem will get solved if you start eating solid food | Risk of looser and more frequent bowel movements. | Risk of looser and more frequent bowel movements |
| 12 | Use of NSAID | Can still take Non-steroidal anti-inflammatory drugs (NSAID) | There is a risk of developing ulcers, especially with NSAID or tobacco use. | Patients must avoid non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen. | Patients must avoid non-steroidal anti-inflammatory drugs (NSAIDs. |
| 13 | Estimated weight loss | There is a loss of about 60% of excess body weight (EBW). | The estimated body weight loss is 70-80% in 1 -2 yrs. | 60 to 80 percent of their excess body weight over 2 years. | Patients lose an average of 85% of their excess body weight. It is associated with the highest percentage of weight loss. |
Which One of the Bariatric Surgeries is Best For You?
Some bariatric surgeries are not suitable for all obese patients but should be considered for obese patients at high risk of morbidity and mortality. Also, people who have not achieved adequate weight loss with lifestyle and medical management and who are suffering from the complications of obesity. Bariatric surgeries can result in substantial weight loss, resolution of comorbid conditions, and improved quality of life.
In making the right surgical choice, the concept of shared decision-making (SDM) is adopted. In SDM, at least the doctor and the patient should participate together, the doctor presents the empirical information of various dispositions, while the patient presents their individual preferences and values, and this information exchange and discussion will achieve the best possible treatment options
When choosing any of the bariatric surgeries, the main concerns on people’s minds are viz:
- Out-of-Pocket Costs
The average cost of bariatric surgery can range from $14,000 to more than $30,000 with an average of $23,000. But the cost depends on several factors viz: the type of surgery chosen, the Hospital and the surgeon providing the services. Other costs considered are:
-
- Pre-op Costs
- Consultations with the nutritionist and/or dietitian.
- Associated psychological visits for your required mental health clearance.
- Cardiologist (heart health clearance).
- Lab work, echocardiogram (ECG or EKG) and/or costs for X-Rays.
- Surgeon’s initial consultation fee.
- Cost for a sleep study.
- Cost During Surgery
- The costs associated with the hospital stay.
- Surgical fees.
- Anesthesia.
- Operating room.
- Any necessary assistant staff that will be present during your procedure.
- A pathologist to review biopsies or a radiologist to review x-rays could have additional costs if the need arises.
- Post-Operative Costs
- Reviewing surgical complications, if necessary.
- Visits to the doctor.
- Any necessary vitamins.
- Additional spending on food since healthy food is often more expensive.
- Gym or personal training fees.
- A new wardrobe (you should allow yourself to hit your projected plateau weight first).
- Surgical procedure to get rid of sagging skin.
- Pre-op Costs
- How much weight can be lost?
- Risk of complications.
- Side effects.
- Recovery time.
It is estimated that about 40% of all bariatric procedures might undergo some form of re-operation, a reversal and or conversion.

The gastric sleeve can be associated with insufficient weight loss /weight regain as a short or long complication. Conversion of the primary gastric sleeve to a duodenal switch or Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S) may be considered if you’ve already had a sleeve gastrectomy and aren’t happy with the results.
This is reserved for patients with insufficient weight loss, weight regains or for complications such as gastroesophageal reflux disease (GERD), leaks or strictures that fail to resolve by medical or endoscopic procedures.
The Gastric Sleeve is also ideal for patients who do not want to deal with malabsorption or do not need to lose more than 130 pounds(81.6 kg) while the Gastric bypass is ideal for those patients who need to lose up to 150 plus pounds(68kg ) rapidly and who are diabetic with high blood pressure, high cholesterol, arthritis, heart burns or sleep apnea– often get better quickly.
For even greater and faster weight loss than a gastric bypass can provide, the Biliopancreatic Diversion should be considered. If one has had abdominal surgery before, simpler surgeries might not be possible.
The SADI is particularly beneficial for diabetic patients and has the highest resolution in type 2 diabetes. It is also beneficial for super-obese patients and has a lower risk of long term weight regain.
It is a good revisional procedure for weight regain after sleeve gastrectomy as the sleeve can often be left untouched and just connected to the distal bypass reducing the operation time and the need for the revision of the sleeve.
Conclusion
Bariatric surgeries are excellent options to help achieve healthy, long-term weight loss and improve medical conditions related to obesity. While all operations have risks, bariatric procedures performed at accredited centres are safe and have a low risk for complications.
Successful bariatric surgery requires a team-based approach including the surgeon, dietitian, psychologist, nurse case manager, and obesity medicine specialist who will focus on taking you through each step of the journey.
Patients will do better if they continue to eat healthily, engage in physical activity, keep their appointments with obesity medicine providers, and take vitamins and mineral supplements as instructed.
Lifelong monitoring by a multidisciplinary team is very essential.

