Appendicitis is a condition caused by inflammation of the vermiform appendix. The vermiform appendix is the anatomical name for the appendix. It means worm-like appendage.
It is the blind distal end of the large caecum (the first part of the colon) with normal tubal layers and is considered by most to be a vestigial organ and is present only in humans, certain anthropoid apes and the wombat.
At birth, the appendix is short and broad at its junction with the caecum, but differential growth of the caecum produces the typical tubular structure by about the age of 2 years.
The appendix varies considerably in length and circumference with an average length of between 7.5 and 10 cm. Under the microscope, the lumen of the vermiform appendix is irregular, being encroached upon by multiple longitudinal folds of the mucous membrane.
Crypts are present but are not numerous and at the base of the crypts lie cells called the argentaffin cells (also known as the Kulchitsky cells), which may give rise to cancer cells called carcinoid tumours. The appendix is the most frequent site for carcinoid tumours, which may present with appendicitis due to occlusion of the appendiceal lumen.
The sub mucous layer has very many prominent lymphatic tissues in the appendix of young adults, which seems to be important in the aetiology of appendicitis.
What is Acute Appendicitis?
Appendicitis is a condition that results when the vermiform appendix gets inflamed. This can be of 2 types:
-
Acute Appendicitis
This is simply an acute inflammation of the appendix. It is one of the main causes of acute abdomen in the ER.
Acute appendicitis is relatively rare in infants, and becomes increasingly common in childhood and early adult life, reaching a peak incidence in the teens and early 20s. After middle age, the risk of developing appendicitis is quite small. The incidence of appendicitis is equal among males and females before puberty. In teenagers and young adults, the male-female ratio increases to 3:2 at age 25; thereafter, the greater incidence in males declines.
-
Chronic Appendicitis
Chronic appendicitis is a rare medical condition and can be very difficult to diagnose because the symptoms may come and go, and they can also be mild. The most common symptom is abdominal pain.
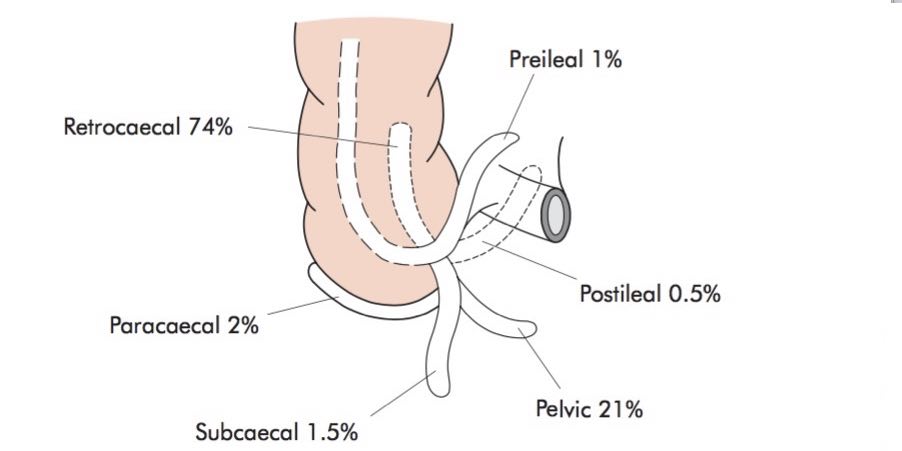
Locations of the Appendix (see diagram below)
The appendix is usually a right-sided organ, usually in the right lower quadrant of the abdomen but can sometimes be on the left abdomen in a rare condition called Dextro rotation, here the organs change positions with the liver and appendix on the left and the spleen and the heart on the right.
However, the appendix position is in relation to the gut viz:
-
Retrocaecal 74% (the appendix lies behind the caecum)
Rigidity is often absent, and even application of deep pressure may fail to elicit tenderness (called silent appendix), the reason being that the caecum distended with gas prevents the pressure exerted by the hand from reaching the inflamed structure.
-
Pelvic 21% (the appendix lies in the pelvis)
Occasionally, early diarrhoea results from an inflamed appendix being in contact with the rectum. When the appendix lies entirely within the pelvis, there is usually a complete absence of abdominal rigidity, and often tenderness over McBurney’s point is also lacking.
This is the maximal point of tenderness in appendicitis. It is the junction of the middle and outer thirds of the line joining the umbilicus to the anterior superior iliac spine. In some instances, deep tenderness can be made out just above and to the right of the symphysis.
-
Paracaecal 2%
The Appendix is lateral to the cecum and the ascending colon.
-
Subcaecal 1.5%
The location of the appendix is under the caecum
-
Preileal 1%
The appendix here is located anterior-superior to the terminal ileum
-
Postileal 0.5%
In this case, the inflamed appendix lies behind the terminal ileum. It presents the greatest difficulty in diagnosis because the pain may not shift, diarrhoea is a feature and marked retching may occur. Tenderness, if any, is ill-defined, although it may be present immediately to the right of the umbilicus.
The Pathology of Appendicitis
This is obstruction. Since the appendix is a tube, so obstruction can be from viz:
- Fecolith (‘poop rock’)
This is a hardening of faeces into lumps of various sizes and can occur anywhere in the intestinal tract if found in the appendix it is also called appendicolith or a Fecolith.
- Undigested seeds
Foreign bodies are known to constitute a cause of appendicitis and among the plethora of possible objects is a seed, which is the third most frequent (about 0.05% of appendectomies).
- Intestinal parasites (pinworms)
Parasites can find their way into the appendix thus causing mechanical obstruction.
- Lymphoid follicle overgrowth (also called lymphoid hyperplasia)
There is a dense collection of lymph nodes that get to maximum size near the appendix in children and adolescents causing an obstruction. Their growth can be in response to viral infection or even immunization.
As the appendix is plugged up, the appendix mucosa usually secretes mucus and fluid, just like the other guts to moisten it and also to keep pathogens from entering the bloodstream, as the secretions build-up:
- The pressure in the appendix increases and this compresses the visceral nerve fibres leading to abdominal pain.
- The gut flora (E.coli &Bacteroides fragile) now has time to multiply greatly, and the body’s immune system responds with white cell build-up seen in the lab as increased white blood cell count (WBC). The patients also respond by developing a fever, abdominal pain and nausea /vomiting.
- As the pressure build-up continues, the blood supply to the appendix becomes compromised leading to ischemia and in a small percentage of people, the appendix ruptures.
- With rupture of the appendix, the bacteria escape to the peritoneal cavity leading to widespread peritonitis, rebound tenderness and guarding.
- The danger of peritonitis is the development of an abscess around the appendix called the periappendiceal abscess.
Symptoms / Signs of Acute Appendicitis
The classic acute appendicitis symptoms are:
- Epigastric, periumbilical pain (pain around the umbilicus) followed by brief nausea, vomiting, and anorexia. After a few hours, the pain shifts to the right lower quadrant and increases with cough and motion.
Classic signs of appendicitis are
- Right lower quadrant Pain.
- Rebound tenderness is located at the McBurney point.
- Right lower quadrant pain with palpation of the left lower quadrant (Rovsing sign),
- An increase in pain is caused by passive extension of the right hip joint that stretches the iliopsoas muscle (psoas sign).
- Pain caused by passive internal rotation of the flexed thigh (obdurate sign).
- Low-grade fever (rectal temperature 37.7 to 38.3° C [100 to 101° F]) is common.
Unfortunately, these classic findings appear in less than 50% of patients. Many variations of appendicitis symptoms and signs occur. Pain may not be localized, particularly in infants and children. Tenderness may be diffuse or in rare instances absent. Bowel movements are usually less frequent or absent; if diarrhoea is a sign, a retrocecal appendix should be suspected.
Red or white blood cells may be present in the urine. Atypical symptoms are common among older patients and pregnant women, in particular, pain is less severe and local tenderness is less marked.
Diagnosis of Appendicitis
-
Clinical evaluation
The diagnosis of acute appendicitis is essentially clinical however, a decision to operate based on clinical suspicion alone can lead to the removal of a normal appendix in 15–30% of cases.
-
Clinical and laboratory-based scoring systems
Several clinical and laboratory-based scoring systems have been devised to assist in diagnosis. The most widely used is the Alvarado score
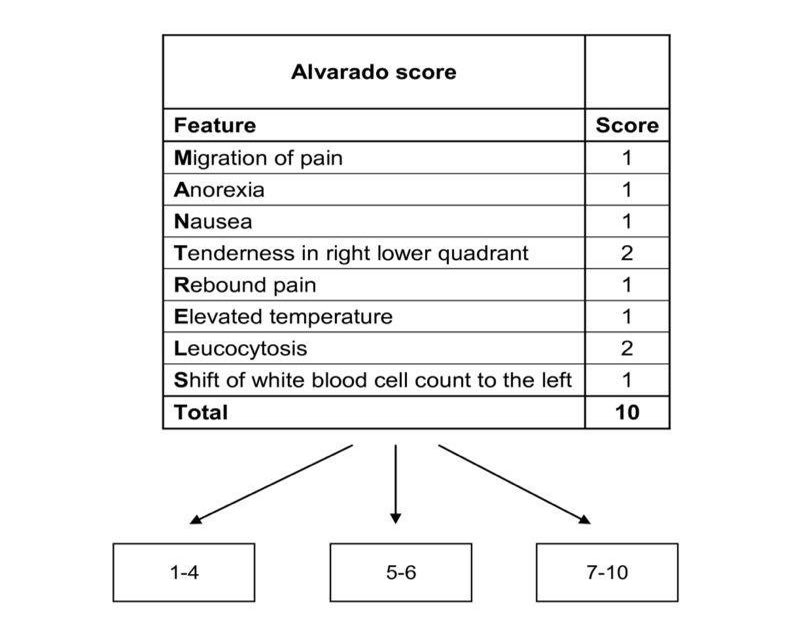
A score of 7 or more is strongly predictive of acute appendicitis.
In patients with an equivocal score (5–6), abdominal ultrasound or contrast-enhanced CT examination further reduces the rate of negative appendicectomy.
-
Abdominal CT if necessary
In patients with atypical or equivocal findings, imaging studies should be done without delay. Contrast-enhanced CT has reasonable accuracy in diagnosing appendicitis and can also reveal other causes of an acute abdomen.
-
Ultrasonography is an option for CT
Abdominal ultrasound examination is more useful in children and thin adults, particularly if gynaecological pathology is suspected, with a diagnostic accuracy of over 90%.
-
Laparoscopy
Can be used for diagnosis as well as the definitive treatment of appendicitis. It may be especially helpful in women with lower abdominal pain of unclear aetiology.
Appendicitis Treatment
-
Surgical removal of the appendix
Treatment of acute appendicitis is an open or laparoscopic appendectomy because treatment delay increases mortality, a negative appendectomy rate of 15% is considered acceptable. The surgeon can usually remove the appendix even if perforated. Occasionally, the appendix is difficult to locate: In these cases, it usually lies behind the cecum or the ileum and mesentery of the right colon.
-
- Open surgery
A cut or incision of about 2 to 4 inches long is made in the lower right-hand side of the abdomen and the appendix is taken out through the incision.
-
- Laparoscopic surgery
This method is less invasive i.e. a small incision is used.1-3 tiny cuts are made and a long tube called the laparoscope is put into one of the cuts. The laparoscope has a video camera and surgical tools. The surgeon looks at the monitor and guides the tools and the appendix is removed with this instrument.
-
IV fluids and antibiotics
Third-generation cephalosporins are the preferred antibiotics of choice. For non-perforated appendicitis, no further antibiotics are required. If the appendix is perforated, antibiotics should be continued for 4 days. Also, the patient should be given intravenous fluids.
If surgery is impossible, antibiotics although not curative markedly improve the survival rate.
Complications of Appendicitis
-
Peritonitis
If the appendix ruptures, the lining of the abdomen called the peritoneum gets infected with bacteria.
-
Abscess
Sometimes pus forms around the appendix. This is called appendiceal abscess and it results when the body tries to fight infection. It is very rare and occurs in 1 in 500 cases and can be a complication of the surgery itself.
The pus can be drained using ultrasound guidance and antibiotics are given. An appendectomy may be postponed for some months. This is called an interval appendectomy.
-
Appendix stump appendicitis
The stump of an improperly removed appendix can still get inflamed and cause symptoms of acute appendicitis.
Conclusion
Appendicitis is a surgical emergency because it can rupture within 48-72 hours of symptoms onset with resultant life-threatening sequelae. Variations in the position of the appendix, age of the patient and degree of inflammation make the clinical presentation notoriously inconsistent but the early presentation to the hospital can make the difference.

