Acne vulgaris is a common skin condition that affects most people at some point. It is most frequent among adolescents and young adults but is not limited to these ages.
The severity of skin involvement varies from minimal involvement to disfiguring and highly inflammatory presentations. Hyperpigmentation, scarring, and negative psychosocial effects are common complications.
Sebaceous glands produce a substance called sebum, which is responsible for keeping the skin and hair moisturized. During adolescence, sebaceous glands enlarge and produce more sebum under the influence of hormones called androgens.
This abnormal serum level changes the activity of the usually harmless bacteria, Cutibacterium acnes, which becomes more aggressive and causes inflammation and pus.
The hormones also thicken the inner lining of the hair follicle causing blockage of the pores and thus causing Acne Vulgaris.
What is Acne Vulgaris?
Acne vulgaris is the medical name for common acne- the presence of blackheads, whiteheads, and other types of pimples on the skin.
Types of Spots
There are 6 main types of spots caused by acne vulgaris viz:
- Blackheads
They are small black or yellowish bumps that develop on the skin. The black colour produced by the inner lining of the hair follicle gives it a blackhead appearance.
- Whiteheads
Whiteheads have a similar appearance to blackheads, but are firmer and will not empty when squeezed.
- Papules
These are small red bumps that may feel tender or sore.
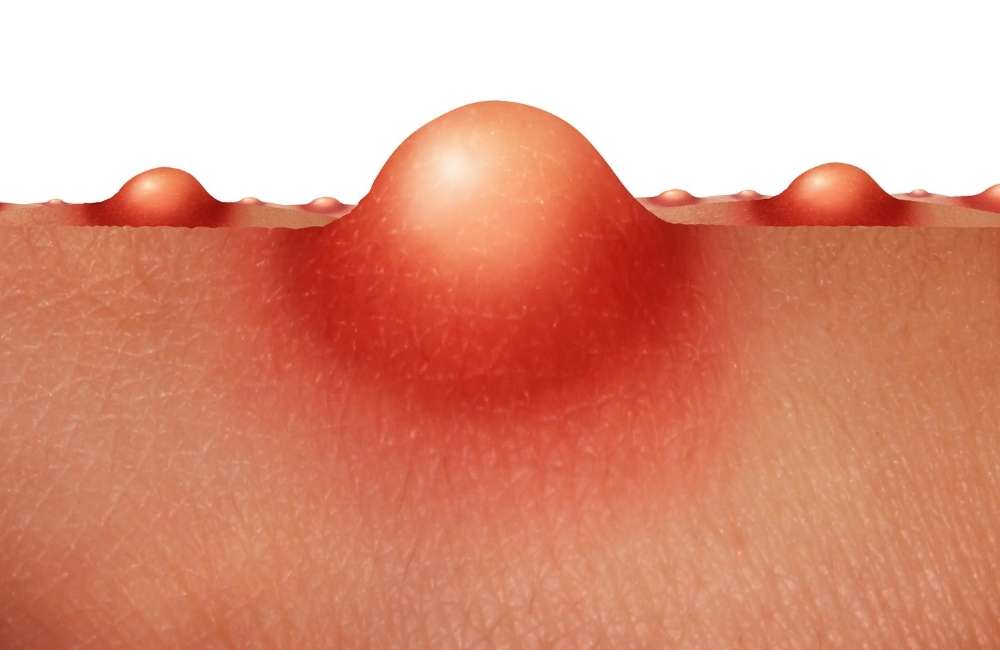
- Pustules
Similar to papules, but have a white tip in the centre, caused by a build-up of pus.
- Nodules
Large hard lumps build up beneath the surface of the skin and can be painful.
- Cysts
The most severe type of spot caused by acne; they’re large pus-filled lumps that look similar to boils but rarely form deep abscesses and carry the greatest risk of causing permanent scarring which manifests as tiny and deep pits (icepick scars), larger pits, shallow depressions, or hypertrophic scarring or keloids.
Classification of Acne Vulgaris
-
Noninflammatory
It is characterised by the presence of comedones; sebaceous plugs impacted within follicles. They are termed open or closed depending on whether the follicle is dilated or closed at the skin surface. Plugs are easily extruded from open comedones but are more difficult to remove from closed comedones. Closed comedones are the precursor lesions to inflammatory acne.
-
Inflammatory
It is characterised by the presence of papules, pustules, nodules, and cysts.
Causes of Acne Vulgaris
Acne vulgaris is caused by a combination of multiple factors viz:
-
Excess Sebum Production
During puberty, a hormone called androgen increases and this causes the sebaceous glands to produce more of the oily substance, sebum. Typically sebum and dead skin cells come up through the hair follicles and out through the pores in the skin. When sebum, skin cells, and bacteria clog the follicles, the sebum can’t escape through the pores thus causing acne.
As one enters early adulthood, these hormones may decrease enough that acne will start to disappear. In about 40% of women, acne may continue into their 40s because of hormonal changes and other causes including:
-
- Hormonal changes in pregnancy or from the menstrual cycle.
- Some medications (Examples include drugs containing corticosteroids, testosterone or lithium).
- Occlusive cosmetics, cleansers, lotions, and clothing.
- High humidity and sweating.
- Polycystic ovarian syndromes(PCOS).
-
Follicular Plugging with Sebum and Keratinocytes
With excessive sebum production in the adolescent period, follicular plugging and hyper-proliferation of keratinocytes result.
-
The colonisation of follicles by Cutibacterium acnes
Cutibacterium acnes (formerly known as Propionibacterium acnes) is a normal human anaerobe. When C. acnes colonize closed comedones, it breaks down sebum into free fatty acids. This irritates the follicular epithelium and starts an inflammatory response by white blood cells (Neutrophils and lymphocytes) and this further disrupts the epithelium.
The inflamed follicle ruptures into the dermis (sometimes precipitated by physical manipulation or harsh scrubbing), where the comedone contents elicit a further local inflammatory reaction, producing papules. If the inflammation is intense, grossly purulent pustules occur.
-
Release of multiple inflammatory mediators
Acne Vulgaris Myths
These factors have little effect on acne:
- Chocolate and greasy foods
Eating chocolate or greasy food has little to no effect on acne.
- Hygiene
Acne isn’t caused by dirty skin. Scrubbing the skin too hard or cleansing it with harsh soaps or chemicals irritates the skin and can make acne worse.
- Cosmetics
Cosmetics don’t necessarily worsen acne, especially if you use oil-free makeup that doesn’t clog pores (noncomedogenic) and remove makeup regularly. Non-oily cosmetics don’t interfere with the effectiveness of acne drugs.
Risk factors for Acne Vulgaris
The risk factors include:
- Age
People of all ages can get acne, but it’s most common in teenagers.
- Hormonal changes
Such changes are common during puberty or pregnancy.
- Family history
Genetics plays a role in acne. If both of your parents had acne, you’re likely to develop it too.
- Greasy or oily substances
You may develop acne when your skin comes into contact with oil or oily lotions and creams.
- Friction or pressure on your skin
This can be caused by items such as telephones, cellphones, helmets, tight collars and backpacks.
Symptoms of Acne Vulgaris

Acne signs vary depending on the severity of the condition:
- Whiteheads (closed plugged pores).
- Blackheads (open plugged pores).
- Small red, tender bumps (papules).
- Pimples (pustules), which are papules with pus at their tips
- Large, solid, painful lumps under the skin (nodules)
- Painful, pus-filled lumps under the skin (cystic lesions)
- Acne usually appears on the face, forehead, chest, upper back and shoulders.
Diagnosis of Acne Vulgaris
Diagnosis of acne vulgaris is by examination and the following are assessed.
- Contributing factors (e.g., hormonal, mechanical, or drug-related
- The severity of the acne (mild, moderate, severe
- Psychosocial impact.
Treatment Options for Acne Vulgaris
It is important to treat acne to reduce the extent of disease, scarring, and psychological distress. Treatment of acne involves a variety of topical and systemic agents directed at reducing sebum production, comedone formation, inflammation, and bacterial counts and at normalizing keratinization.
-
Mild Acne Treatment
Treatment of mild acne should be continued for 6 weeks or until lesions respond. Maintenance treatment may be necessary to maintain control and treatment can either be single-agent therapy or dual therapy.
- Single-agent therapy
This is generally sufficient for comedonal acne. A mainstay of treatment for comedones is daily topical tretinoin as tolerated. Alternatives for patients who cannot tolerate topical tretinoin include
-
- Daily Adapalene gel.
- Tazarotene cream or gel.
- Azelaic acid cream, and glycolic or Salicylic acid.
Adverse effects include erythema, burning, stinging, and peeling.
- Dual therapy
A combination of tretinoin with benzoyl peroxide, a topical antibiotic, or both should be used to treat mild papulopustular (inflammatory) acne. The topical antibiotic is usually erythromycin or clindamycin. Combining benzoyl peroxide with these antibiotics may help limit the development of resistance. Treatments have no significant adverse effects other than drying and irritation (and rare allergic reactions to benzoyl peroxide.

- Physical extraction of comedones
Extraction of comedones with a comedone extractor is an option for patients unresponsive to topical treatment. Comedone extraction may be done by a physician, nurse, or physician assistant. One end of the comedone extractor is like a blade or bayonet that punctures the closed comedones while the other end exerts pressure to extract the comedones.
- Oral antibiotics
Antibiotics like tetracycline, minocycline, doxycycline and erythromycin can be used when the wide distribution of lesions makes topical therapy impractical.
- Clascoterone
Clascoterone is the first topical androgen receptor inhibitor for the treatment of acne. It can be used in patients 12 years of age and older. Clascoterone 1% cream is applied 2 times a day. Adverse effects include redness, scaling or dryness, and itching.
-
Moderate Acne Treatment
Oral systemic therapy with antibiotics is the best way to treat moderate acne. Antibiotics effective for acne include tetracycline, minocycline, erythromycin, doxycycline and sarecycline (a new tetracycline antibiotic). Full benefit takes more than 12 weeks.
Topical therapy for mild acne is usually used concomitantly with oral antibiotics. Doxycycline and minocycline are first-line drugs; both can be taken with food at a dosage is 50 to 100 mg orally 2 times a day.
Doxycycline may cause photosensitivity while minocycline may have more adverse effects with chronic use, including drug-induced lupus and hyperpigmentation.
Long-term use of antibiotics may cause gram-negative pustular folliculitis around the nose and in the centre of the face. This uncommon superinfection may be difficult to clear and is best treated with oral isotretinoin after discontinuing the oral antibiotic.
In women, prolonged antibiotic use can cause candida vaginitis. If local and systemic therapies do not eradicate this problem, antibiotic therapy for acne must be stopped.
If the patient is female and unresponsive to oral antibiotics, a trial of oral antiandrogens (oral contraceptives and/or spironolactone may be considered.
-
Severe Acne Treatment
Oral isotretinoin is the best treatment for patients with moderate acne in whom antibiotics are unsuccessful and for those with severe inflammatory acne. Dosage is usually
- 1 mg/kg once a day for 16 to 20 weeks,
- The dosage may be increased to 2 mg/kg once a day.
- If adverse effects make this dosage intolerable, it may be reduced to 0.5 mg/kg once a day.
After therapy, acne may continue to improve, thus many patients do not require a 2nd course of treatment. When needed, however, it is resumed only after the drug has been stopped for 4 months, except in severe cases when it may be resumed earlier.
This drug is nearly always effective, but use is limited by adverse effects, including:
- Dryness of conjunctivae and mucosae of the genitals.
- Chapped lips.
- Arthralgia( mostly of the large joints or lower back)
- Depression/Suicide
- Elevated lipid levels.
- Risk of birth defects if treatment occurs during pregnancy.
Hydration with water followed by petrolatum application usually alleviates mucosal and cutaneous dryness. The following investigations must be done before starting this treatment and a repeat reassessment done within 4 weeks of treatment commencement unless abnormalities are noted viz:
- Complete blood count (CBC)
- Liver function tests (LFT)
- Lipid profile (triglyceride, and cholesterol levels).
- Pregnancy tests should be done before the commencement of therapy and monthly until 1 month after therapy stops.
Because this drug is teratogenic (the ability of a drug to cause fetal abnormalities or deformities), women of childbearing age are required to use 2 methods of contraception for 1 month before, during and after treatment and continue for at least 1 month after stopping treatment.
For cystic acne, intralesional injection (within the lesion) of 0.1 mL triamcinolone acetonide suspension 2.5 mg/mL. Please note that the 10-mg/mL suspension must be diluted. This has a quick clinical improvement with reduced scarring.
Local atrophy may occur but is usually transient. For isolated, very boggy lesions, incision and drainage are often beneficial but may result in residual scarring.
Another form of acne viz:
Pyoderma faciale is treated with oral corticosteroid and isotretinoin. Acne fulminans is commonly treated with oral corticosteroids and systemic antibiotics.
Acne conglobata is treated with oral isotretinoin and systemic corticosteroids if severe and if systemic antibiotics fail.
For acne caused by endocrine abnormalities (e.g., polycystic ovary syndrome, virializing adrenal tumours in females), antiandrogens are indicated. Spironolactone which has some antiandrogen effects is sometimes prescribed to treat acne at a dose of 50 to 150 mg (maximum 200 mg) orally once a day.
Scarring
Small scars can be treated with chemical peels, laser resurfacing, or dermabrasion. Deeper, discrete scars can be excised. Wide, shallow depressions can be treated with subcision (subcutaneous incision-less surgery) or injection of collagen or another filler. Fillers, including collagen, hyaluronic acid, and polymethylmethacrylate, are temporary and must be repeated periodically.
Role of diet
Specific changes in diet are not recommended to treat acne, but developing information indicates that acne may be related to a high glycemic index and limited data indicate that some dairy, especially skim milk, can worsen acne. There is insufficient evidence to endorse recommendations related to antioxidants, probiotics, and fish oil.
Conclusion
Acne cannot be cured but can be treated. The following self-help measures may be helpful.
- Affected skin areas should be washed with mild soap or cleanser and lukewarm water. Very hot water can make the acne worse and washing should not be done more than 2 times a day as this can irritate the skin and worsen the symptoms.
- Blackheads should not be cleaned and spots squeezed to avoid permanent scarring.
- The use of too much makeup, skincare products and cosmetics should be avoided. Skincare products labelled water-based non-comedogenic are recommended and also remember to completely remove all make-up before going to bed.
- Hair falling across the face should be prevented
- And last but not least, consult your GP.

